can an overshot jaw correct itself supplier

This website is using a security service to protect itself from online attacks. The action you just performed triggered the security solution. There are several actions that could trigger this block including submitting a certain word or phrase, a SQL command or malformed data.
An overbite might not seem like a serious condition for your dog, but severely misaligned teeth can lead to difficulty eating, gum injuries and bruising, bad breath and different types of dental problems, including tooth decay and gingivitis. Fortunately, there are ways to help fix the problem before it becomes irreversible.
An overbite is a genetic, hereditary condition where a dog"s lower jaw is significantly shorter than its upper jaw. This can also be called an overshot jaw, overjet, parrot mouth, class 2 malocclusion or mandibular brachynathism, but the result is the same – the dog"s teeth aren"t aligning properly. In time, the teeth can become improperly locked together as the dog bites, creating even more severe crookedness as the jaw cannot grow appropriately.
This problem is especially common in breeds with narrow, pointed muzzles, such as collies, shelties, dachshunds, German shepherds, Russian wolfhounds and any crossbred dogs that include these ancestries.
Dental examinations for puppies are the first step toward minimizing the discomfort and effects of an overbite. Puppies can begin to show signs of an overbite as early as 8-12 weeks old, and by the time a puppy is 10 months old, its jaw alignment will be permanently set and any overbite treatment will be much more challenging. This is a relatively narrow window to detect and correct overbites, but it is not impossible.
Small overbites often correct themselves as the puppy matures, and brushing the dog"s teeth regularly to prevent buildup can help keep the overbite from becoming more severe. If the dog is showing signs of an overbite, it is best to avoid any tug-of-war games that can put additional strain and stress on the jaw and could exacerbate the deformation.
If an overbite is more severe, dental intervention may be necessary to correct the misalignment. While this is not necessary for cosmetic reasons – a small overbite may look unsightly, but does not affect the dog and invasive corrective procedures would be more stressful than beneficial – in severe cases, a veterinarian may recommend intervention. There are spacers, braces and other orthodontic accessories that can be applied to a dog"s teeth to help correct an overbite. Because dogs" mouths grow more quickly than humans, these accessories may only be needed for a few weeks or months, though in extreme cases they may be necessary for up to two years.
If the dog is young enough, however, tooth extraction is generally preferred to correct an overbite. Puppies have baby teeth, and if those teeth are misaligned, removing them can loosen the jaw and provide space for it to grow properly and realign itself before the adult teeth come in. Proper extraction will not harm those adult teeth, but the puppy"s mouth will be tender after the procedure and because they will have fewer teeth for several weeks or months until their adult teeth have emerged, some dietary changes and softer foods may be necessary.
An overbite might be disconcerting for both you and your dog, but with proper care and treatment, it can be minimized or completely corrected and your dog"s dental health will be preserved.
To achieve strong oral health and a wonderful smile, your upper and lower jaws need to evenly meet. This allows you to do things like eating and swallowing with ease and avoid some very serious health risks to your jaw, mouth and teeth.
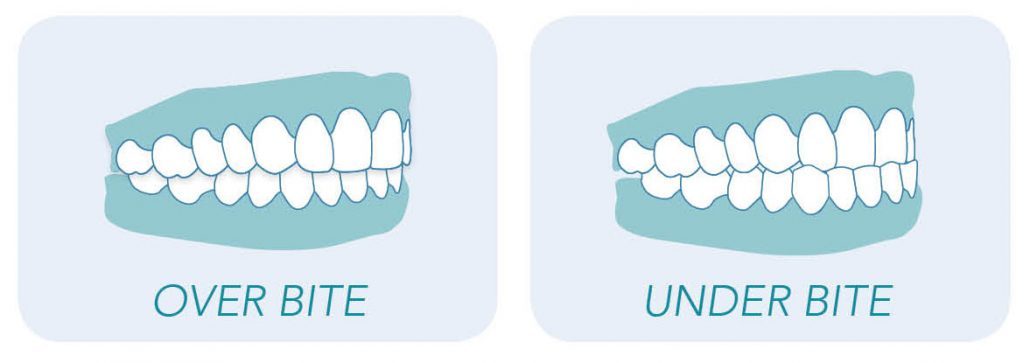
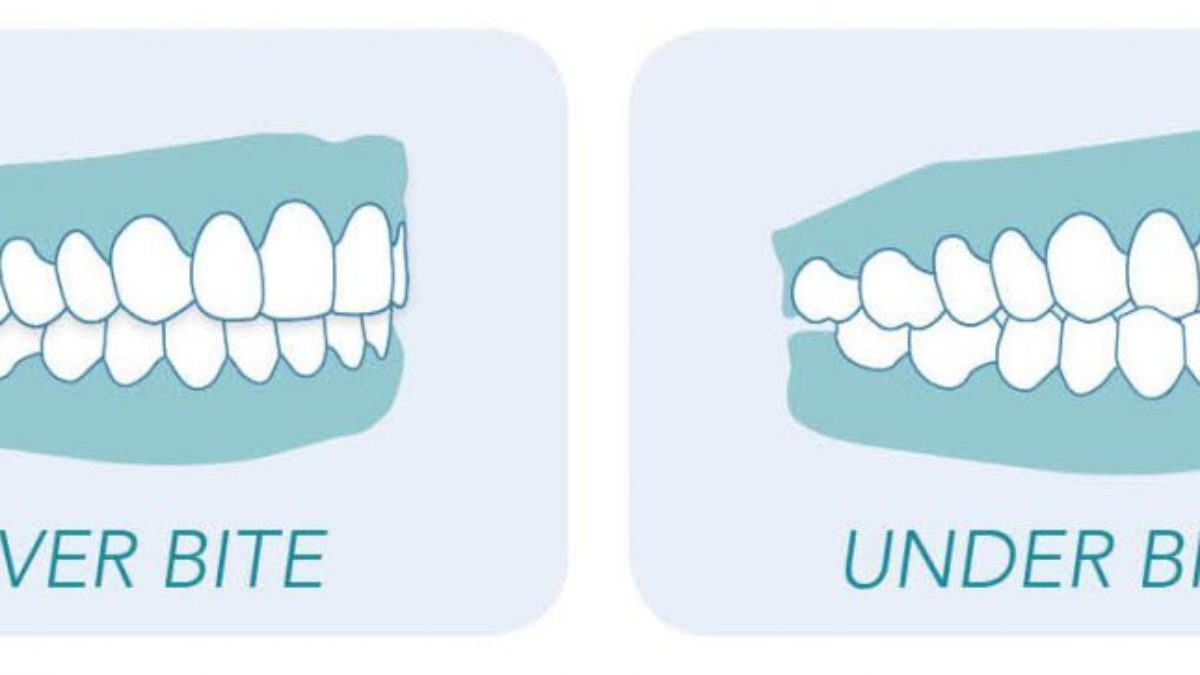
A malocclusion is whenever the upper and lower rows of teeth do not meet. There are three types of malocclusions: overbites, underbites and crossbites. Overbites and underbites are the most common but all three require immediate and thorough orthodontic treatment. It can be tricky to know if you have a severe enough overbite or underbite to warrant orthodontic intervention.
How do you go about fixing your overbite or underbite? How do the treatments differ? What can you expect from the various treatments? As you can imagine, there are a lot of questions that you need answered. To start, let’s review the basics of identifying overbites and underbites. Then, we’ll explore treatment options and the best courses of action with respect to dealing with your malocclusion before the problem worsens.
Just because your upper teeth extend somewhat over your lower teeth, doesn’t necessarily mean you have an overbite. In addition, minor overbites are very common and might not require braces. Overbites that are severe enough to need fixing occur when the upper teeth overlap the bottom teeth to an excessive degree of roughly 4 to 10 millimeters. This can be caused by genetics, a recessive chin, misaligned bites, thumb sucking, poorly fitted crowns, gum disease or as the result of injury. Also, sometimes teeth just come in awkwardly.
Overbites are more common than underbites and are called a Class II bite. One thing to remember is that having a slight overbite is normal because the shape of the human skull naturally allows for the upper teeth to extend beyond the lower teeth. During checkups, your dentist should measure your overbite and underbite and consult with you if they suspect any issues.
The good news is that overbites are considered to be easily treatable using conventional methods. It is easier to fix in young children so don’t hesitate to speak with an orthodontist immediately about your child or children’s potential malocclusion. It’s never too late to fix this issue if the patient is willing.
An underbite, a Class III bite, is when the lower teeth extend beyond the upper. Essentially, the lower jaw protrudes, making it impossible for the lower row of teeth to align with the upper row causing the potential for several serious oral health issues. This can be caused by the upper jaw bone being underdeveloped or the bone in the lower jaw being overdeveloped.
Like overbites, underbites can begin during childhood due to behaviours like thumb-sucking or caused by genetics or as the result of an accident. Whatever the cause, severe underbites should be treated immediately as to avoid the potential hazards that can surface over time.
Most people believe there are only two malocclusions. There is a third type, though, known as a crossbite. And while it is less common, it still requires diagnosis and treatment. Crossbite is a lateral misalignment meaning the top teeth are positioned too close to the cheek or tongue.
Crossbite occurs during childhood and doesn’t naturally correct itself over time. It can occur between the front or back teeth. The side effects are similar to and just as serious as overbites and underbites. Upon diagnosis, your dentist should present treatment options and recommend a course of action.
While you can do a remedial check to see if you exhibit the signs of having a misaligned bite, this is a job best left to your dentist or orthodontist. They will conduct an inspection that looks for:
There are also mental health and self-esteem risks associated with overbites and underbites. This is often overlooked but our appearance can inform how we feel and determine our emotional state. We believe that dentistry should help you feel confident and comfortable with your smile.
For less severe bites, a removable retainer is a suitable enough solution to produce the desired results. This type of retainer hooks around the back teeth to hold itself securely in place. The removable element makes it easier to clean your teeth but the patient must be responsible enough to remember to put it in every day. Forgetting for long stretches would negate this treatment’s effectiveness.
The most common way to treat misaligned bites is with braces or aligners, especially with children or teenagers. Braces use taut wires to connect tiny brackets to apply consistent pressure to teeth. This forces them to realign and straighten over time. Braces have a high success rate but can be pricy and patients must wear them for anywhere between one to three years.
If you need more incentive to deal with a misaligned bite early, keep in mind that insurance providers often cover braces for children but not adults. We always recommend speaking with your insurance provider to discuss your coverage and payment options.
Some cases of misaligned bites only require aligners. Popular options like Invisalign, which are clear and removable, work wonders while allowing people to go about their day with minimal interruption or embarrassment. Invisalign isn’t an appropriate solution for every case of malocclusion so ask your dentist if they make sense for your situation.
Treatment duration depends on the severity of your issue but be prepared to commit for several months if not a year or two. It might sound as if treatment will upend your life but it is worth it for both your oral health and the smile you will achieve and get to show off every day. Your dentist should be well equipped to talk you through the emotional impact of these procedures and help prepare you for any changes to your daily life.
Don’t wait and let your overbite, underbite or crossbite worsen and create additional issues for your mouth, teeth and gums. Letting these problems linger can result in you needing caps, crowns or dental hardware installed. Furthermore, neglect can make them harder to fix down the road.
We hope this article has answered some of your questions about overbites and underbites. If you or your child needs treatment, then remember just about any misaligned bite can be repaired. It’s always better to tackle the problem head-on and immediately.

Most people aren’t born with perfectly aligned teeth. Usually, slightly misaligned teeth don’t require any medical treatment. However, correcting an underbite, especially when it’s severe, can have big benefits.
Teeth will become easier to clean. Your risks for tooth decay and gum disease will decrease. You’ll also feel less strain on your teeth, jaws, and facial muscles.
This can reduce your risks of breaking a tooth and also painful symptoms of temporomandibular disorders, which are common with underbites. Some common treatments for underbite include:
Brushing and flossing your teeth regularly in addition to visiting a dentist for checkups and cleanings are important parts of treatment for healthy teeth. But those with an underbite or other dental issues must take special care of their teeth to prevent further damage and decay.
Brush your teeth at least twice a day for two minutes each time with toothpaste containing fluoride. Pay attention to brushing along your gumline and on the inside, outside, and the back of your mouth. Be sure you floss in addition to brushing. See your dentist at least twice a year for checkups and cleanings.
Medical treatment is the only way to truly correct an underbite and align teeth correctly. At the very least, medical treatment can improve the appearance of an underbite.
In less severe cases of underbite, a dentist may be able to use wire or plastic braces or other dental appliances to move the teeth into their correct place.
Removal of one or more teeth on the lower jaw may also help improve the appearance of an underbite if overcrowding of the teeth is contributing to the issue. A dentist may also use a grinding device to shave down or smooth teeth that are large or stick out.
The earlier an underbite is addressed, the better. If a child’s underbite is less severe, parents should wait until at least age 7 to seek corrective treatment such as braces. That’s when permanent teeth begin to erupt.
If your child has a severe underbite, especially if it’s caused by a birth defect such as cleft lip, early surgery may help. Talk to your child’s dentist and doctor to see what course of treatment they recommend.
Surgery has its risks and should only be used in children when underbite is interfering with their quality of life or ability to eat, breathe, or speak.
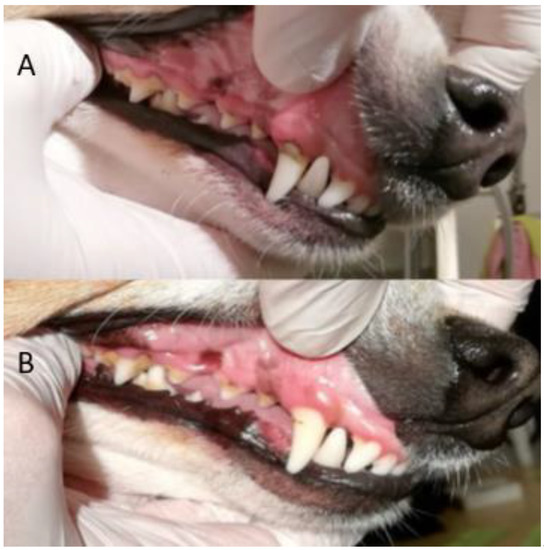
Normally, a puppy will have 28 baby teeth once it is six months old. By the time it reaches adulthood, most dog breeds will have 42 teeth. A misalignment of a dog"s teeth, or malocclusion, occurs when their bite does not fit accordingly. This may begin as the puppy"s baby teeth come in and usually worsens as their adult teeth follow.
The smaller front teeth between the canines on the upper and lower jaws are called incisors. These are used to grasp food and to keep the tongue inside the mouth. Canines (also known as cuspids or fangs) are found behind the front teeth, which are also used to grasp. Behind the canines are the premolars (or bicuspids) and their function is to shear or cut food. Molars are the last teeth found at the back of the mouth and they are used for chewing.
If problems with the palate persist, a fistula may result and become infected. In cases of misaligned teeth (or malocclusion), the dog may have difficulty chewing, picking up food, and may be inclined to eat only larger pieces. They are also prone to tartar and plaque build-up.
The tips of the premolars (the teeth right behind the canines) should touch the spaces between the upper premolars, which is called the scissor bite. However, it is normal for flat-faced breeds (brachycephalic) such as Boxers, Shih Tzus, and Lhasa Apsos not to have scissor bites.
With an overbite, the upper jaw is longer than the lower one. When the mouth is closed, a gap between the upper and lower incisors occurs. Puppies born with an overbite will sometimes have the problem correct itself if the gap is not too large. However, a dog"s bite will usually set at ten months old. At this time improvement will not happen on its own. Your pet"s overbite may worsen as the permanent teeth come in because they are larger and can damage the soft parts of the mouth. Teeth extractions are sometimes necessary.
The way the upper teeth align with the lower teeth is called occlusion. It is normal for most breeds to have a slight overlap of the upper front teeth. When the jaw is closed, the lower canine (fang) should fit in front of the upper canine. Most cases of malocclusion have a hereditary link.
Most bite malocclusions do not require treatment. In some cases, extractions may be necessary. It’s a good idea to brush the teeth regularly to prevent abnormal build-up of tartar and plaque. Your veterinarian will sometimes recommend a dental specialist if you want to correct the teeth misalignment. In recent years, “braces” have been made for puppies to realign the teeth.
An underbite is a fairly common problem for children. With a normal bite, your child’s upper teeth stick out slightly farther than their lower teeth when they bite down. With an underbite, however, the lower teeth actually protrude out farther than the upper teeth.
The University of Maryland Medical Center identifies genetics as the most common cause of underbite. Some children are simply born with a natural tendency for an underbite. If you had an underbite as a child, there is a good chance your son or daughter will have the same issue.
Thumb sucking, constantly pushing one’s tongue against teeth, and extended use of a pacifier can also contribute to an underbite. But these factors are much less common than simple genetics.
Underbites are problematic because they do not look “normal.” It can make others think you are conveying an emotion that you aren’t trying to convey, which can be socially awkward, especially for children.
Not only that, but underbites can also cause difficulties with chewing and eating, excessive jaw pain (such as TMJ), challenges with speaking, tooth decay because of worn down enamel, sleep apnea, snoring, and difficulty sleeping.
Because of the many complications, it is recommended that an underbite is treated as soon as possible. Fortunately, there are several treatment options available, which we will now explore.
There are several treatment options and they tend to vary based off the severity of the underbite. One of the reasons we recommend children visit the orthodontist by age 7 is that the earlier treatment begins, the simpler and less expensive it will be.
For some children, a simple appliance is all that is required. An upper jaw expander is a wire-frame device that we place across the child’s palate. Each night, you use a special key to widen the jaw expander a very small amount. Over time, this process causes the upper jaw to widen until there is no longer an underbite. Patients typically wear this appliance for about a year, followed by a retainer that helps hold the teeth in place.
This is another appliance, although it is slightly more complicated. It resembles headgear because it wraps around your child’s head. It uses metal bands fastened to the upper back teeth, and then pulls the upper jaw back into the correct position.
When an appliance won’t do the trick, braces probably will. Braces are the most common way to correct an underbite. Braces are made up of several components, but essentially they involve brackets bonded directly to the front of a tooth. Brackets hold the wires that move teeth in the correct position.
Braces can also include spacers or separators that create space between teeth; the rubber ties that hold the wire to the brackets; and rubber bands that attach to the brackets of both the upper and lower teeth to apply pressure and create a perfect bite.
In rare cases of extreme underbite, surgery might be required. We rarely recommend surgery and avoid it as much as possible. Treating an underbite early will help ensure treatment is easy and does not require surgery.
If your child has an underbite and you are in the Cumming, Hamilton Mill, or Suwanee, Georgia areas, then we recommend you make an appointment with us at Chattahoochee Family Orthodontics. Our team of orthodontists have extensive experience and love working with children.
Each child is unique so we will start by determining the severity of the underbite and then create a treatment plan that suits the specific needs of your child. Remember, leaving an underbite untreated can cause further complications down the road, so don’t delay!

Undershot is a class III malocclusion that is also referred to as mandibular prognathism, maxillary brachygnathism, mandibular mesioclusion, or an underbite. This malocclusion is characterized by a shorter upper jaw and a longer lower jaw, resulting in lower teeth that are in front of the upper teeth. While this condition is normal for some breeds, such as Bulldogs, in many breeds it is unusual. An undershot jaw occurs when the lower jaw grows faster than normal and becomes longer than the upper jaw, and is usually evident around 8 weeks of age in puppies. This misalignment can cause soft tissue trauma, such as to the lips. When the incisors meet instead of fitting next to each other, it is called a level bite. When the malocclusion causes the lower incisors to be placed in front of the upper incisors, it is called a reverse scissors bite.
The cause of overshot and undershot jaws in dogs relate to the increased or decreased rate of growth of the upper and lower jaws in relation to one another. This can occur due to a: Genetic disorder Trauma; Systemic infection ;Nutritional disorder; Endocrine disorder; Abnormal setting of puppy teeth; Early or late loss of puppy teeth.
After a quick physical exam, your vet may have to sedate your dog in order to perform a thorough oral exam. This will assess your dog’s skull type and teeth location in relation to the teeth on the opposite jaw. Often, the placement of the upper and lower incisors in relation to one another can determine what type of malocclusion your dog has. Your vet will note any areas of trauma due to teeth striking those areas, and any cysts, tumors, abscesses, or remaining puppy teeth that may be present. A dental X-ray can also help to assess the health of the jaws and teeth. These diagnostic methods will lead to a diagnosis of an overshot or undershot jaw in your dog.
Treatment of a jaw misalignment will depend on the severity of the condition. If your dog has a misalignment, but can still bite and chew food without problems, no treatment may be needed. If the misalignment is caught early in a puppy’s life, it may only be temporary and may correct itself over time. However, there are times when intervention may be needed. If your puppy’s teeth are stopping the normal growth of his jaws, then surgery to remove those puppy teeth may be performed. This may allow the jaws to continue to grow, but will not make them grow. For older dogs who are experiencing pain and trauma due to misaligned jaws and teeth, oral surgery is generally performed to extract teeth that are causing trauma, to move teeth so that they fit, or to create space for a misaligned tooth to occupy. Other therapies include crown reductions or braces.
If your dog is genetically programmed to have an overshot or undershot jaw, intervention can help, but will not slow or stop the abnormal growth of either jaw. Prevent jaw misalignments in puppies by not breeding dogs who have overshot or undershot jaws.

This website is using a security service to protect itself from online attacks. The action you just performed triggered the security solution. There are several actions that could trigger this block including submitting a certain word or phrase, a SQL command or malformed data.
This website is using a security service to protect itself from online attacks. The action you just performed triggered the security solution. There are several actions that could trigger this block including submitting a certain word or phrase, a SQL command or malformed data.
Infants with recessed jaw/ retrognathia present with unique feeding challenges and are sometimes misdiagnosed with ankyloglossia or tongue tie. This is of particular concern, because in some cases a frenulectomy is contraindicated. Although the anterior maxillary and mandible alignment is impacted, the primary concern is the tongue sitting posteriorly toward the pharynx. In severe cases airway obstruction can occur but milder cases also require consideration for airway patency. These babes often present with stridor reflective of increased respiratory effort but when paired with a confirmed diagnosis of laryngeal or tracheal malacia adequate respiratory support needed for sustained energy and coordination for feeding are frequently compromised.
The discrepancy between the maxilla and mandible often cause the nipple and areola to compress with anterior rotation. The position of the tongue can also inhibit elevation and retraction of the posterior tongue needed to recreate adequate inner oral pressure during the suck needed to efficiently draw milk from the breast. These oral mechanics can cause irritation to the nipple or tissue trauma or they have difficulty transitioning off of nipple shields sometimes mistaken as characteristic of ankyloglossia (tongue-tie). Many babes have improved latch in this position as gravity assists with tongue and occasionally jaw forward.
Detection of a recessed jaw can be a bit challenging. Infants naturally have a slightly recessed chin/jaw as part of normal development; however, those that present with a gap of 3 mm or more between the anterior upper and lower gum line often struggle at breast. These infants sometimes have prominent chins with a horizonal crease between the mental region and the lower lip. The lower lip often rests tucked behind the upper lip or superior alveolar ridge. Observation at breast and bottle will also reveal increased facial tension particularly along the lateral orbicularis oris often resulting in a narrow latch as the babe tries to compensate for anterior rotation of the nipple between the upper and lower gum lines. In more involved cases the infant struggles with the extension reflex of the tongue needed for latch stability as gravity pulls the back of the tongue posteriorially.
The good news is that positioning adjustments have proven very helpful, particularly at breast to use gravity to move the tongue anteriorly in the mouth creating additional pharyngeal space. For babies without sternal precautions or poor respiratory endurance I suggest a trial with Mom reclined with babe in prone position (also known as tummy to tummy, laid back or biological position). I find most success with placing a rolled bath towel or narrow end of the Gia or breast feeding pillow at babe’s chest allow them to come down onto the nipple without head extension. The breastfeeding pillow can also provide support through the baby’s hips as they rest in a tucked position in the center of the pillow with the lower inside edge supporting their bottom. It is not uncommon to hear less stridor in this position as a result.
For bottle feeding, elevated side lying with slight anterior rotation at the hips) or high cradle (with hips slightly forward, not directly under the shoulders) can work nicely. These positions also provide nice support for respiration. I personally prefer placing babe in classic football hold but rotate their hips and shoulders so they are “stacked” which also places the babe at a nice angle with space for the bottle and supports lots of yummy eye contact/engagement.
When bottle supplementation is needed, the Playtex Drop In Nurser with the Natural Latch nipple provides nice support along the jaw when the bottle is held at a slight angle to allow the lower edge of the nipple along the lower lip. I typically prefer this bottle/nipple for breast feeding infants to match the gape/latch that compliments oral positioning at the breast. Infants with small gaps between the maxilla and mandible typically show no concerns for breathing. However, infants with wide gaps require careful monitoring. If an infant demonstrates any stress responses in supine, parents report concern for potentially obstructive noises during sleep or the young infant spontaneously moves themselves from their back to side lying a sleep study and/or airway patency assessment should be done by an otolaryngologist (ENT). The infant’s pediatrician needs to be aware of these concerns for consideration of positioning for sleep.Some pediatricians may consider elevated or side lying sleep positioners specifically designed for these purposes. These should only be used under the direction of the physician.
The majority of infants with a slightly recessed jaw outgrow these feeding concerns. At around 3-4 months of age the infant’s neck elongates and the pharynx deepens as the jaw moves forward with facial growth. This brings the posterior tongue slightly forward with increased space allowing for functional tongue elevation and retraction. At this point most infants can transition to more traditional breastfeeding positions.
Allyson served on the Financial Planning Board of the American Speech-Language-Hearing Association. She is a past president of the Oregon Speech-Language-Hearing Association. She has served on the advisory board and as an adjunct professor at Portland State University for 19 years and is a guest lecturer in Pacific University and University of Oregon graduate programs. She has also traveled nationally and taught as a member of the Education Resources clinical faculty. Allyson was recently awarded the Honors of the Association by the Oregon Speech-Language-Hearing Association.

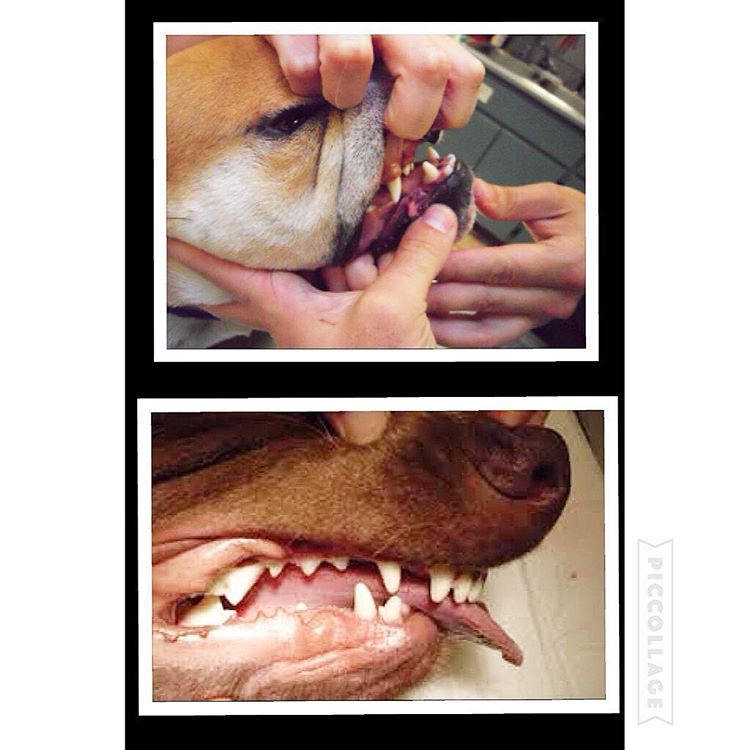
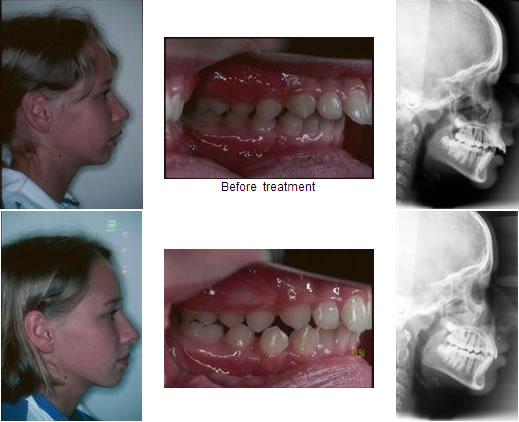
Here is a visual look into what an “undershot” and “overshot” jaw looks like. In recent years, I’ve noticed more and more dogs with this issue. Can a dog live productive life with a malocclusion: (imperfect positioning of the teeth when a jaws closed) Yes but with some issues along the way.
Let’s begin with a puppy will have 28 “puppy teeth” by the time it reaches six months old (this number can vary from breed to breed) By adulthood, most breeds will have a total of 42 teeth. As defined above a malocclusion or simply a misalignment of a dog’s teeth occurs when their bite does not fit accordingly beginning as puppy’s teeth come in and worsening as their adult teeth follow.
the upper jaw is longer than the lower one, an overshot or overbite. When a dogs mouth is closed, a gap between the upper and lower incisors (teeth) will be present. In most cases, puppies are born with a slight over/under bite and with time the problem can correct itself if the gap is not too large. What should be noted is if a dog’s bite remains over/undershot by 8-10 months old, that’s how it will remain for the remainder of its life. In overbite’s the structure may worsen as the permanent teeth come in as they are larger and can damage the soft parts of the mouth. Teeth extractions are sometimes necessary.
Structural dentition of a puppies jaw should be checked very early on to help eliminate this issue. Unfortunately most dog owners won’t notice until is late in the game. More so is the issues of backyard and/or inexplicable breeders breeding dogs with undershot/overshot jaws and potentially passing along this trait to future generations.
With an overbite, the upper jaw is longer than the lower one. When the mouth is closed, a gap between the upper and lower incisors occurs. Puppies born with an overbite will sometimes have the problem correct itself if the gap is not too large. However, a dog’s bite will usually set at ten months old. At this time improvement will not happen on its own. Your pet’s overbite may worsen as the permanent teeth come in because they are larger and can damage the soft parts of the mouth. Teeth extractions are sometimes necessary.
Problems that can arise from malocclusion are; difficulty chewing, picking up food and other objects, dogs with overshot jaws tend to pick up larger chunks of food since they can’t chew nor pick up smaller morsels which can lead to choking and future intestinal issues. These dogs are also prone to tartar and plaque build up which if left untreated can lead to other significant health issues such as heart problems. Other issues are listed below:
What’s important to note is that most malocclusions do not require treatment, it’s simply how a dog will live its full life as. This is important since most breeders breeding for financial gains don’t think about. What can be done is to brush the teeth regularly to prevent abnormal build-up of tartar and plaque. A veterinarian in cases that can be solved will sometimes recommend a dental specialist if a client want to correct the teeth misalignment. Recently I’ve heard o specialist putting “braces” on puppies to realign the teeth.
#dog #dogs #puppy #pup #puppies #puppylove #pets #life #family #bulldog #maltese #mastiff #chihuahua #cockerspaniel #vet #meds #instadog #instagood #instadaily

Enzo is the Hawthorne Hills Veterinary Hospital Pet of the Month for May. Everyone knows that puppies need vaccines to keep them healthy and protected from diseases. However, it can be easy to underestimate the benefits of thorough and regular examinations when puppies are growing into adulthood. Every breed has special characteristics that make them unique and add to their appeal and sometimes there are physical changes that need to be addressed quickly. For this reason our veterinarians believe in examinations with every vaccine, especially during a puppy’s formative months.
Enzo is a short-haired Havanese and he was born with his lower jaw shorter than the upper jaw. This is called an Overbite, also referred to as an Overshot Jaw, a Parrot Mouth or Mandibular Brachygnathism. This malocclusion is a genetic change and can be seen in a number of breeds, oftentimes collie related breeds and dachshunds. Occasionally this change happens because of differences in the growth of the upper and lower jaws, and in many cases it doesn’t cause any significant problems other than cosmetically.
Dr. Robin Riedinger evaluated Enzo at his first visit when he was just 11 weeks of age and while the lower jaw was too short, there was no evidence of damage and no indication that this was causing a problem for Enzo. When there is abnormal occlusion of the teeth, it is important to monitor closely for trouble caused by the teeth being aligned improperly. Malocclusions can lead to gum injuries, puncturing of the hard palate, abnormal positioning of adjacent teeth, abnormal wear and bruising of the teeth, permanent damage and subsequent death of one or more teeth, and in the long run, premature loss of teeth. Some malocclusions can be severe enough to interfere with normal eating and drinking.
Within three weeks, when Enzo was only 3.5 months old, it was clear that our doctors would need to intervene. The left and right sides of Enzo’s upper jaw (maxilla) were growing at different rates because the lower canine teeth were being trapped by the upper canine teeth. This is called Dental Interlock. Because the teeth are ‘locked’ in place, the lower jaw cannot grow symmetrically and this creates a number of other problems. Early intervention is critical.
The solution for Dental Interlock is to extract the teeth from the shorter jaw; in this case, the lower ‘baby’ canines and thereby allow the lower jaw (mandible) to grow in the best way possible. This procedure is most effective when the Dental Interlock is discovered early and the extractions are performed quickly. In some cases, this can be as early as ten weeks of age. Dr. Riedinger consulted with a local veterinary dental specialist to confirm the treatment plan and to get advice on extracting the deciduous teeth without damaging the developing adult canines. Dental radiographs are essential to proper extraction technique and also to ensure that there are no other abnormalities below the gumline.
You can see how long the roots of the deciduous ‘baby’ teeth are. During normal growth, the body will begin to resorb the roots, making them loose, and allow them to fall out as the adult tooth begins to emerge. When we need to remove the deciduous teeth before they are loose, it can be quite tricky to remove the tooth carefully without breaking it and without injuring the adjacent teeth.
Once extracted, each deciduous canine tooth was about 2 centimeters long; the roots were about 1.5 centimeters. Many people are surprised to learn that the root of a dog’s tooth is so large – 2/3 to 3/4 of the tooth is below the gumline. This is one reason why it is so important to use radiographs to evaluate teeth on a regular basis, not just in a growing puppy. Adult teeth can, and frequently do, have problems that are only visible with a radiograph.
Enzo came through his procedure extremely well. He was given pain medications for comfort and had to eat canned foods and avoid chewing on his toys for the next two weeks to ensure that the gum tissue healed properly. As he continues to grow we will be monitoring how his jaw develops and Dr. Riedinger will also be watching the alignment of his adult canine teeth when they start to emerge around six months of age. Hopefully this early intervention will minimize problems for Enzo in the future.
This website is using a security service to protect itself from online attacks. The action you just performed triggered the security solution. There are several actions that could trigger this block including submitting a certain word or phrase, a SQL command or malformed data.

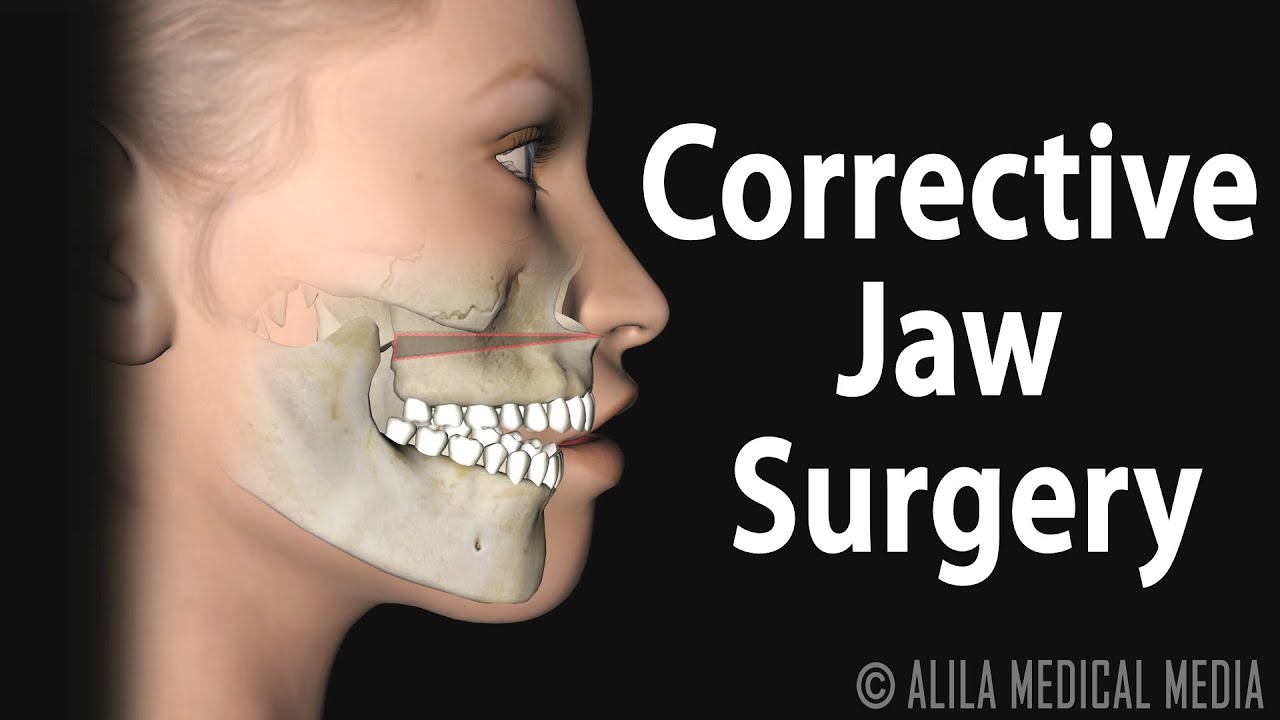
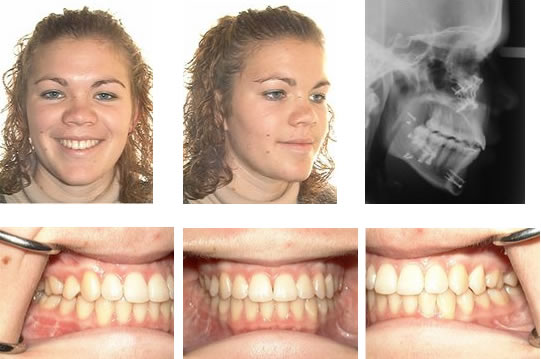
The term bad bite is a lay term for malocclusion. What that means is that the teeth of the upper jaw or maxilla do not align appropriately with the teeth of the lower jaw or mandible. A malocclusion can be limited to the teeth themselves and would be fixed commonly with orthodontic treatment or braces. A malocclusion can also be the result of misalignment of the jaws themselves. This can be either congenital, meaning from birth, developmental in nature, or from a traumatic injury.
The surgery used to correct a severe malocclusion from a misaligned jaw is called orthognathic surgery. This includes procedures to move the upper jaw or maxilla forward, backward, or even to widen it. It also includes procedures to move the lower jaw or mandible rotationally to correct asymmetry, forward or backward. Orthognathic surgery is usually completed in conjunction with orthodontic treatment or braces.
Most of the time your orthodontist will be the one to refer you to a surgeon to discuss jaw surgery. At times adjunctive procedures are completed to ensure symmetry and harmony of the facial profile, which can include chin surgery or genioplasty as well as cheek augmentation or malar implants.
When considering orthognathic surgery the materials that are used to secure the jaws or maxilla and mandible into the new position are titanium plates and screws. They are very strong with a low profile so that they will not affect your appearance, but will maintain the new position of the bones during the healing phase. Due to the strength most of the time the teeth do not need to be left wired together after surgery. The hardware or plates and screws that are used to position the jaws during surgery a most often left in place for life and are not removed.
In general, people are not allergic to surgical-grade titanium. That is not to say, however, that one could not be allergic to titanium though it would be very rare.
Recovery after orthognathic jaw surgery is relatively rapid though may vary by patient and specific procedure. In general it will involve an overnight stay in the hospital with discharge in the morning or afternoon the day following your surgery. The diet is limited to liquids for the first few days, and is advanced to a non-chew diet for the first four weeks. A soft-chew diet is then gradually advanced to a normal diet after six weeks of healing.
Though rare, if the teeth are wired together after surgery, a liquid diet would be required for six weeks after surgery. Typically one week off of work or school is required after surgery. Activity is restricted for the first four weeks with no lifting greater than 40 lbs. After four weeks, light activities can be resumed with low impact. Contact sports and rigorous activities can be resumed after 12 weeks or three months following surgery.
There are many ways to wire the teeth or jaws together. The term we use is maxillo-mandibular fixation or MMF for short. Though it is rare in conjunction with orthognathic surgery if required the orthodontic appliances or braces that the patient has on are used. Wires can be looped around the braces of the upper and lower teeth to wire the jaw shut.
The jaw may be wired shut due to trauma or mandibular fractures as well in order to immobilize it. It may also be wired for reconstructive purposes. This is typically done with either arch bars or Ivy loops.
An arch bar is a temporary brace that has hooks on it that can be secured to the teeth with wires. Once in place on the upper and lower teeth, the hooks are used to loop wires around that are used to wire the jaw shut.
Lastly, there are screw retained arch bars. This means that rather than securing the arch bar to the teeth with wires it is screwed into the bone of the maxilla and mandible. It too has hooks on it that can be used to loop wires around to wire the jaw shut.
The functionality of wiring the jaws or teeth together serves to immobilize the bones while they are healing, therefore acting like a cast. We ask patients who are wired together to carry wire cutters with them in case they are involved in an accident. It is usually not necessary for patients to cut their own wires.
With most orthognathic surgery or jaw surgery to move the maxilla and mandible, it is not necessary to wire the teeth together. Instead, we use titanium plates and screws as mentioned previously to secure the jaw into the new position. Occasionally, with very large movements or in the event of a less than ideal fracture the teeth or jaws may be wired together in order to immobilize the bones during the initial phase of healing. This is not very common.
The use of maxillo-mandibular fixation or MMF is not painful. The use of local anesthetics, conscious sedation, and occasionally general anesthesia make the process quite comfortable. After the completion of the procedure there can be some discomfort with the wires in the mouth, though this is usually very minor and can be managed with wax in sharp areas, the same as for traditional braces or orthodontic appliances.
When undergoing orthognathic surgery or corrective jaw surgery the majority of the incisions are hidden inside the mouth. The oral mucosa or gum tissue has an amazing capacity to heal and even intraoral scarring is minimal. Oftentimes, the application of the titanium screws in the mandible once in the new position, can require a small incision near the angle of the jaw. It is typically no larger than 2-4 mm and is usually not noticeable after three to six months.
If you are considering surgery for a severe misalignment of the teeth or jaws, first and foremost, you should visit an orthodontist. Correction of a malaligned, underdeveloped, or overdeveloped jaw requires a combined effort, usually including an orthodontist and an oral and maxillofacial surgeon.
Oral and maxillofacial surgeons have special training that requires extensive knowledge of facial surgery as well as dentistry, which makes them well equipped to manage surgery involving correction of a bad bite while also considering overall facial harmony. I would recommend relying on your orthodontist for ultimate referral though seeking care initially from an oral and maxillofacial surgeon is reasonable as well. The surgeon will likely provide a referral to a local orthodontist.
Following jaw surgery, we typically prescribe a mild analgesic in combination with a non-steroidal anti-inflammatory drug or NSAID like ibuprofen. With upper jaw surgery, we often give a nasal decongestant to decrease swelling of the nasal mucosa. In regards to antibiotics, an intravenous dose is provided pre-operatively and is continued post-operatively until discharge on a regular schedule. On discharge from the hospital your surgeon may recommend a short course of oral antibiotics.
A moderate amount of swelling is expected with orthognathic surgery. In order to limit the amount of swelling and improve patient comfort we utilize high-dose perioperative steroid administration. This includes an oral dose the evening prior to surgery followed by intravenous dosing in the operating room and post-operatively while in the hospital. The amount of swelling will vary from patient to patient. Typically after two weeks it is vastly improved and by four to six weeks it is 90 percent resolved. It may take up to six months for the last 10 percent of swelling to resolve, though this is typically only noticed by the patient and close family.
The incidence of infection following orthognathic or jaw surgery is very low. In the literature, the incidence is reported to be between 6 and 15 percent. These figures are high, in our opinion. When it occurs, the infection is easily treated with antibiotics and drainage with minimal discomfort and no long-term effects.
During jaw surgery, we utilize high-dose perioperative intravenous antibiotics for prophylaxis to prevent infection. Meticulous surgical technique and accomplishing the surgery in an efficient manner will also reduce infection rates. Occasionally, if bone grafts are utilized during surgery, we will continue the antibiotic therapy for seven to ten days orally after discharge. Our patients are also sent home with an antibacterial mouth rinse to help keep the wounds clean and are instructed on meticulous oral hygiene practices. Proper oral hygiene post-operatively is important in reducing the bacterial load in the mouth and adjacent to the surgical wounds.
Following an orthognathic surgery, we have patients return for numerous postoperative visits in order to ensure proper healing. We typically see patients at one week, four weeks, six weeks, and 12 weeks following surgery. We also see the patient back at the six-month and 12-month intervals once the orthodontic therapy is complete and the braces have been removed. A final set of records is obtained at that time. Close post-operative follow-up is important in order to catch any possible complications early as well as to ensure the proper bite and jaw position has been obtained and is stable.
JRA stands for juvenile rheumatoid arthritis. It is very different from the adult form. It is often a diagnosis of exclusion meaning all other diagnoses are ruled out. It can involve the temporomandibular joints. If so, management typically involves a team approach not only including the oral and maxillofacial surgeon and orthodontist, but rheumatologist and other physicians as well.
When it affects the temporomandibular joints JRA can lead to limited opening and malocclusion or a bad bite and misaligned jaws. It is often managed with newer medications typically guided by the rheumatologist. If the disease remains stable, then surgical correction of the bite can be undertaken by the surgeon and orthodontist with traditional orthognathic surgery. If the disease remains active and refractory to medical management, then total joint replacement of the temporomandibular joints may be necessary.
A cleft lip and/or palate is often associated with a cleft of the alveolus or the tooth bearing segments of the upper jaw or maxilla. The patient usually undergoes several surgeries in the area of the cleft at an early age. Because of this early surgery, the normal growth pattern of the maxilla can be restricted.
It is often necessary to advance the upper jaw when the patient is in the mid to late teens. This can be completed in a single surgery and may also be combined with a lower jaw or mandibular surgery. At times, if the movement is too large to complete in a single surgery, a procedure called distraction osteogenesis may be undertaken to reposition the jaw. This procedure grows the jaw over a period of weeks to achieve the desired position. It is typically reserved for very large discrepancies.
Distraction osteogenesis of the jaws is based on the Ilizarov leg lengthening procedure. In many ways, it is more successful and reliable in the head and neck region versus the extremities because of the ample blood supply found in the head and neck. It is typically reserved for very severe deformities that cannot be corrected in a single surgery.
In the mandible or lower jaw it is at times used to advance and grow the jaw forward in order to open the airway and avoid the need for tracheostomy in infants and children with severe micrognathia (small mandible).
As mentioned previously in the maxilla or upper jaw it is often times used in patients who have undergone cleft lip and palate repairs, which can restrict maxillary growth. This can lead to a more severe misalignment of the jaws. Distraction osteogenesis can be utilized in these cases to grow the jaw over a period of time to correct a more severe discrepancy.
The distraction osteogenesis procedure can take more time than traditional orthognathic surgery. During an initial surgery, devices are placed on the mandible or the maxilla. These devices are then turned twice a day by the patient at home, or in the case of infants by the surgeon in the hospital. This advances or grows the jaw by 1 mm per day. A typical advancement may range from 10-15 mm. That would require up to two weeks of turning. Once the growth is complete the devices are no longer turned and remain in place for about 6-12 weeks to allow the new bone to calcify and heal. After this period a second surgery is undertaken to remove the implanted devices.
Following orthognathic surgery, there will be neurosensory changes. The nerves involved with jaw surgery are not motor, meaning surgery will not affect how your face looks or moves. In the lower jaw, the numbness will include the lower lip, chin, and gum tissue, and in general, this should resolve in about three months. Sometimes neurosensory changes take up to 18 months in an adult to resolve completely.
Occasionally, minor neurosensory changes of the lower lip and chin can be permanent. Permanent numbness following an upper jaw (maxilla) surgery is much less common.




 8613371530291
8613371530291