can an overshot jaw correct itself made in china
Undershot is a class III malocclusion that is also referred to as mandibular prognathism, maxillary brachygnathism, mandibular mesioclusion, or an underbite. This malocclusion is characterized by a shorter upper jaw and a longer lower jaw, resulting in lower teeth that are in front of the upper teeth. While this condition is normal for some breeds, such as Bulldogs, in many breeds it is unusual. An undershot jaw occurs when the lower jaw grows faster than normal and becomes longer than the upper jaw, and is usually evident around 8 weeks of age in puppies. This misalignment can cause soft tissue trauma, such as to the lips. When the incisors meet instead of fitting next to each other, it is called a level bite. When the malocclusion causes the lower incisors to be placed in front of the upper incisors, it is called a reverse scissors bite.
The cause of overshot and undershot jaws in dogs relate to the increased or decreased rate of growth of the upper and lower jaws in relation to one another. This can occur due to a: Genetic disorder Trauma; Systemic infection ;Nutritional disorder; Endocrine disorder; Abnormal setting of puppy teeth; Early or late loss of puppy teeth.
After a quick physical exam, your vet may have to sedate your dog in order to perform a thorough oral exam. This will assess your dog’s skull type and teeth location in relation to the teeth on the opposite jaw. Often, the placement of the upper and lower incisors in relation to one another can determine what type of malocclusion your dog has. Your vet will note any areas of trauma due to teeth striking those areas, and any cysts, tumors, abscesses, or remaining puppy teeth that may be present. A dental X-ray can also help to assess the health of the jaws and teeth. These diagnostic methods will lead to a diagnosis of an overshot or undershot jaw in your dog.
Treatment of a jaw misalignment will depend on the severity of the condition. If your dog has a misalignment, but can still bite and chew food without problems, no treatment may be needed. If the misalignment is caught early in a puppy’s life, it may only be temporary and may correct itself over time. However, there are times when intervention may be needed. If your puppy’s teeth are stopping the normal growth of his jaws, then surgery to remove those puppy teeth may be performed. This may allow the jaws to continue to grow, but will not make them grow. For older dogs who are experiencing pain and trauma due to misaligned jaws and teeth, oral surgery is generally performed to extract teeth that are causing trauma, to move teeth so that they fit, or to create space for a misaligned tooth to occupy. Other therapies include crown reductions or braces.
If your dog is genetically programmed to have an overshot or undershot jaw, intervention can help, but will not slow or stop the abnormal growth of either jaw. Prevent jaw misalignments in puppies by not breeding dogs who have overshot or undershot jaws.

This website is using a security service to protect itself from online attacks. The action you just performed triggered the security solution. There are several actions that could trigger this block including submitting a certain word or phrase, a SQL command or malformed data.

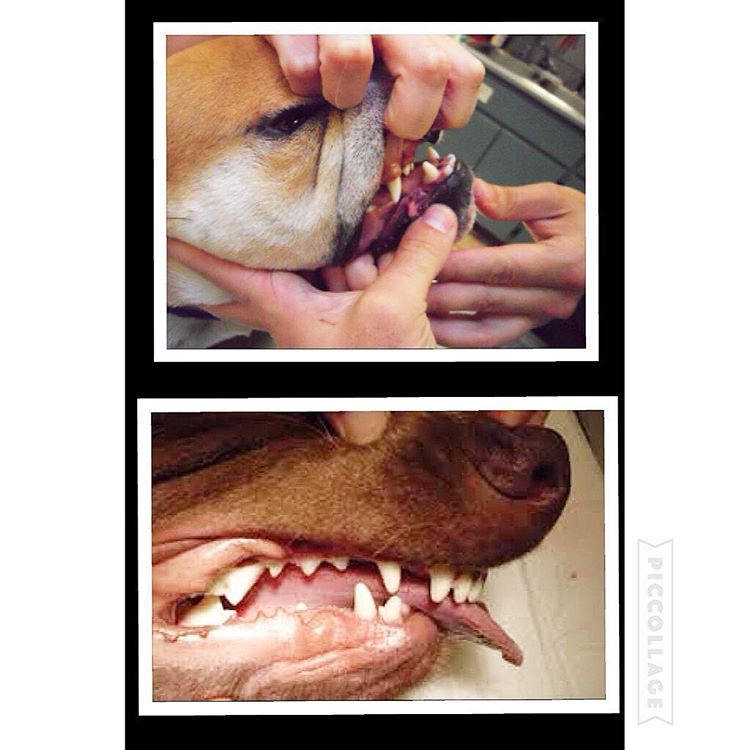
Here is a visual look into what an “undershot” and “overshot” jaw looks like. In recent years, I’ve noticed more and more dogs with this issue. Can a dog live productive life with a malocclusion: (imperfect positioning of the teeth when a jaws closed) Yes but with some issues along the way.
Let’s begin with a puppy will have 28 “puppy teeth” by the time it reaches six months old (this number can vary from breed to breed) By adulthood, most breeds will have a total of 42 teeth. As defined above a malocclusion or simply a misalignment of a dog’s teeth occurs when their bite does not fit accordingly beginning as puppy’s teeth come in and worsening as their adult teeth follow.
the upper jaw is longer than the lower one, an overshot or overbite. When a dogs mouth is closed, a gap between the upper and lower incisors (teeth) will be present. In most cases, puppies are born with a slight over/under bite and with time the problem can correct itself if the gap is not too large. What should be noted is if a dog’s bite remains over/undershot by 8-10 months old, that’s how it will remain for the remainder of its life. In overbite’s the structure may worsen as the permanent teeth come in as they are larger and can damage the soft parts of the mouth. Teeth extractions are sometimes necessary.
Structural dentition of a puppies jaw should be checked very early on to help eliminate this issue. Unfortunately most dog owners won’t notice until is late in the game. More so is the issues of backyard and/or inexplicable breeders breeding dogs with undershot/overshot jaws and potentially passing along this trait to future generations.
With an overbite, the upper jaw is longer than the lower one. When the mouth is closed, a gap between the upper and lower incisors occurs. Puppies born with an overbite will sometimes have the problem correct itself if the gap is not too large. However, a dog"s bite will usually set at ten months old. At this time improvement will not happen on its own. Your pet"s overbite may worsen as the permanent teeth come in because they are larger and can damage the soft parts of the mouth. Teeth extractions are sometimes necessary.
Problems that can arise from malocclusion are; difficulty chewing, picking up food and other objects, dogs with overshot jaws tend to pick up larger chunks of food since they can"t chew nor pick up smaller morsels which can lead to choking and future intestinal issues. These dogs are also prone to tartar and plaque build up which if left untreated can lead to other significant health issues such as heart problems. Other issues are listed below:
What"s important to note is that most malocclusions do not require treatment, it"s simply how a dog will live its full life as. This is important since most breeders breeding for financial gains don"t think about. What can be done is to brush the teeth regularly to prevent abnormal build-up of tartar and plaque. A veterinarian in cases that can be solved will sometimes recommend a dental specialist if a client want to correct the teeth misalignment. Recently I"ve heard o specialist putting "braces” on puppies to realign the teeth.
#dog #dogs #puppy #pup #puppies #puppylove #pets #life #family #bulldog #maltese #mastiff #chihuahua #cockerspaniel #vet #meds #instadog #instagood #instadaily

faces that are associated with the formation of particular varieties and breeds (e.g., Herre and Röhrs 1990; Van Grouw 2018). Well-known examples include Bulldogs, Pugs, and
1990), the investigation of inheritance patterns (e.g., Stockard 1941), the study of genetic underpinnings (e.g., Fondon and Garner 2004; Bannasch et al. 2010; Bertolini et
(domesticated >500 YBP, see text; tree topology is according to Meredith et al. 2011 and Agnarsson and May-Collado 2008). Gray branches indicate species with at least
above 176°, i.e., they are all non-airorhynchic (according to Nussbaumer 1982 and this study, Fig. 1; for data, see Table S1). As we will point out in more detail later,
bones, parts of the snout (premaxilla) are foreshortened and downward tilted (Fig. 1 and Table 1). In other domestic ruminants, such as cattle, no cases of
breeds to be on the small side of the domestic dog body size spectrum (Marchant et al. 2017; Fig. 1G, regression of body size [neurocranium centroid] as the independent
medium-sized and giant breeds, such as the Boxer and Dogue de Bordeaux (Nussbaumer 1982; Marchant et al. 2017). Besides these genetic factors, there is also likely to be
parts of the history of many domestic forms (e.g., dogs [Parker et al. 2017] and chicken [Núñez-León et al. 2019]), this will be notoriously difficult to achieve.
2006; Noden and Schneider 2006; Lwigale and Schneider 2008; Fish and Schneider 2014a; Schneider 2018b). In particular, the use of a unique avian chimeric
along with a shortening of all limbs, is also known from humans (achondroplasia; Parrot 1878; Horton, Hall and Hecht 2007) and has been compared to “bulldog-type”
truncated faces have been found in brachycephalic cats (Schmidt et al. 2017) and genetically engineered mice (Hajihosseini et al. 2001). Such phenotypes in humans are known as a
conformation typically includes a relatively short snout and a large braincase (Bolk 1926; Dechambre 1949; Wayne 1986; Morey 1992; Coppinger and Schneider 1995). Although “pedomorphic” skull proportions pertain
shapes and are particularly prevalent in ponies and miniature horses (Wiggs and Lobprise 1997; Heck, Sánchez-Villagra and Stange 2019). Similarly, the most common
associated with morbidity, e.g., in cats and dogs (see earlier; e.g., Waters 2017; Bessant et al. 2018). Human intervention and medical care are often required for
be less likely to be bred or they will even be killed (Thomson 1996; Alpak et al. 2004; Fischer and Lilje 2011; Smith et al. 2016). Taken together, these points would point to

Underbites may not be the first thing you think of when it comes to dogs, however, there are several breeds sporting this toothy grin. Find out which dogs have underbites and why dogs have underbites in the first place.
Like humans, an underbite in a dog refers to the lower teeth projecting beyond the upper teeth. Veterinarians will refer to this issue as malocclusion. While an underbite can happen in various breeds, it’s commonly seen in brachycephalic breeds.
Shih Tzus are a beloved companion animal commonly found in homes worldwide. These friendly little creatures have a long history of being lap dogs for noble women in China.
Perhaps the dog most commonly associated with an underbite is the English Bulldog. This breed’s predisposal for malocclusion completes the Bulldog’s look. It’s fair to assume if you are purchasing a bulldog, you will have to deal with an underbite.
This is why it’s important to only purchase your English Bulldog from a responsible, ethical, and reputable breeder. A Bulldog with an excessive underbite will not only require expensive dental visits but may experience discomfort while eating.
These lap dogs were bred as companions to royal figures in the Chinese city of Peking. Today, these toy-sized dogs are loved by many. They are regarded as friendly, intelligent, and full of personality.
Pekingese dogs are distinguished by their “lion mane” coat. It’s also not uncommon for these small dogs to present an underbite. Like other brachycephalic breeds, they are prone to having underbites.
It’s not hard to spot a Pug! Their black masked, squished face and fawn shorthair coat set them apart from other dogs. There’s nothing like those little curled tails wagging to greet you!
Like other dogs on this list, Pugs are considered a short skull or brachycephalic breed. With this comes your typical dental problems, including an underbite.
You’re sure to recognize a Boston Terrier. With their smart black and white coat and long bat-like ears, Boston Terriers are beloved by millions. This lively breed has a lot of energy and requires frequent exercise.
This attribute sets it apart from other short-skulled breeds that often prefer a more sedentary lifestyle. These dogs weigh no more than 25 pounds yet love to run, hike, or explore the park. This feature makes them ideal for city dwellers with an active lifestyle.
While they typically come in black and white, Bostons can come in many colors. These include various combinations of brindle, seal, and white. No matter what your Boston Terrier’s coat looks like, there’s a strong likelihood it will have a slight underbite.
While most of the breeds on this list are small dogs, larger breeds such as Boxers also suffer from underbites. Boxers can weigh up to 80 lbs and belong to the working group classification. These dogs are known to be highly intelligent and easily trainable.
According to the AKC breed standard, Boxers have an undershot jaw. The lower jaw should jut forward from the upper and curve upward. These large, athletic, and wrinkly beasts are great companions for individuals and families alike.
These tiny dogs come from Mexico. They are known for having a huge personality trapped in a tiny body! While they may not have a squished face like other breeds on this list, they are a small breed and only reach about 6 lbs on average.
These fluffy little dogs share the homes of millions of people around the world. These dogs originated in Poland and were bred to pull carts, guard livestock, and do other physical jobs. However, they were eventually bred to be smaller to be companion animals.
These long-haired, white, small dogs are very popular. You will typically find Maltese dogs living in urban areas. Their small size has made them ideal city dogs.
However, purebred Maltese often suffer from a variety of dental problems. It’s commonfor a Maltese to display an underbite, ranging from slight to severe.
The first Spaniel to make it on our list, King Charles Spaniels, are a very popular family dog. They rank consistently in the top 20 most popular breeds in the U.S. While most commonly sporting a red and white coat, you can also find King Charles Spaniels to be black and tan and tri-colored.
While known for being friendly and intelligent, King Charles Spaniels are prone to various health issues. The most common health issues are ear infections and dental problems. While these little dogs make fantastic pets, don’t be surprised to find yourself in the veterinarian’s office!
They are sometimes mistaken for a Boston Terrier. While French Bulldogs have been rising in popularity over the past decade, it’s important to understand these dogs commonly exhibit various health problems.
It’s not uncommon for French Bulldogs to have severe underbites. It’s essential to only purchase puppies from reputable breeders that understand genetics.
Severe underbites can result in tooth wear, jaw pain, difficulty eating, or damage to the gums or palette. If your puppy begins to exhibit signs of an underbite, it’s recommended to take them to a veterinarian to see if treatmentis necessary.
Usually, treatment is not necessary. However, there are treatment options if you suspect your dog is experiencing discomfort or pain related to their underbite. Typically, these include extractions, physical therapies, and root canal treatments.
Your local vet is a good place to start! If your dog’s underbite is severe, they will be able to connect you with specialists in your area. Veterinary dentists are specialists that receive extra training to treat oral and dental issues in your pet.
Sometimes, a young dog’s underbite may correct itself. However, it’s most likely that if your puppy is exhibiting an underbite, it will have it throughout its life. This is especially true if you have a brachycephalic or small breed.
If you have a pup with an underbite or are looking at possibly getting one, it’s essential to understand the risk associated with dogs with underbites. While underbites are typically not a problem for most dogs, consult your veterinarian if you’re worried about your dog’s teeth or bite.

An overbite might not seem like a serious condition for your dog, but severely misaligned teeth can lead to difficulty eating, gum injuries and bruising, bad breath and different types of dental problems, including tooth decay and gingivitis. Fortunately, there are ways to help fix the problem before it becomes irreversible.
An overbite is a genetic, hereditary condition where a dog"s lower jaw is significantly shorter than its upper jaw. This can also be called an overshot jaw, overjet, parrot mouth, class 2 malocclusion or mandibular brachynathism, but the result is the same – the dog"s teeth aren"t aligning properly. In time, the teeth can become improperly locked together as the dog bites, creating even more severe crookedness as the jaw cannot grow appropriately.
This problem is especially common in breeds with narrow, pointed muzzles, such as collies, shelties, dachshunds, German shepherds, Russian wolfhounds and any crossbred dogs that include these ancestries.
Dental examinations for puppies are the first step toward minimizing the discomfort and effects of an overbite. Puppies can begin to show signs of an overbite as early as 8-12 weeks old, and by the time a puppy is 10 months old, its jaw alignment will be permanently set and any overbite treatment will be much more challenging. This is a relatively narrow window to detect and correct overbites, but it is not impossible.
Small overbites often correct themselves as the puppy matures, and brushing the dog"s teeth regularly to prevent buildup can help keep the overbite from becoming more severe. If the dog is showing signs of an overbite, it is best to avoid any tug-of-war games that can put additional strain and stress on the jaw and could exacerbate the deformation.
If an overbite is more severe, dental intervention may be necessary to correct the misalignment. While this is not necessary for cosmetic reasons – a small overbite may look unsightly, but does not affect the dog and invasive corrective procedures would be more stressful than beneficial – in severe cases, a veterinarian may recommend intervention. There are spacers, braces and other orthodontic accessories that can be applied to a dog"s teeth to help correct an overbite. Because dogs" mouths grow more quickly than humans, these accessories may only be needed for a few weeks or months, though in extreme cases they may be necessary for up to two years.
If the dog is young enough, however, tooth extraction is generally preferred to correct an overbite. Puppies have baby teeth, and if those teeth are misaligned, removing them can loosen the jaw and provide space for it to grow properly and realign itself before the adult teeth come in. Proper extraction will not harm those adult teeth, but the puppy"s mouth will be tender after the procedure and because they will have fewer teeth for several weeks or months until their adult teeth have emerged, some dietary changes and softer foods may be necessary.
An overbite might be disconcerting for both you and your dog, but with proper care and treatment, it can be minimized or completely corrected and your dog"s dental health will be preserved.

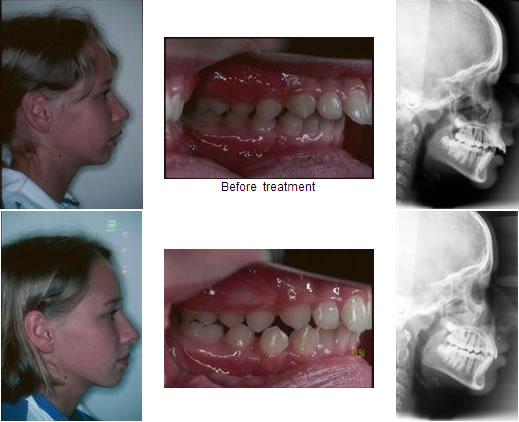
The term bad bite is a lay term for malocclusion. What that means is that the teeth of the upper jaw or maxilla do not align appropriately with the teeth of the lower jaw or mandible. A malocclusion can be limited to the teeth themselves and would be fixed commonly with orthodontic treatment or braces. A malocclusion can also be the result of misalignment of the jaws themselves. This can be either congenital, meaning from birth, developmental in nature, or from a traumatic injury.
The surgery used to correct a severe malocclusion from a misaligned jaw is called orthognathic surgery. This includes procedures to move the upper jaw or maxilla forward, backward, or even to widen it. It also includes procedures to move the lower jaw or mandible rotationally to correct asymmetry, forward or backward. Orthognathic surgery is usually completed in conjunction with orthodontic treatment or braces.
Most of the time your orthodontist will be the one to refer you to a surgeon to discuss jaw surgery. At times adjunctive procedures are completed to ensure symmetry and harmony of the facial profile, which can include chin surgery or genioplasty as well as cheek augmentation or malar implants.
When considering orthognathic surgery the materials that are used to secure the jaws or maxilla and mandible into the new position are titanium plates and screws. They are very strong with a low profile so that they will not affect your appearance, but will maintain the new position of the bones during the healing phase. Due to the strength most of the time the teeth do not need to be left wired together after surgery. The hardware or plates and screws that are used to position the jaws during surgery a most often left in place for life and are not removed.
In general, people are not allergic to surgical-grade titanium. That is not to say, however, that one could not be allergic to titanium though it would be very rare.
Recovery after orthognathic jaw surgery is relatively rapid though may vary by patient and specific procedure. In general it will involve an overnight stay in the hospital with discharge in the morning or afternoon the day following your surgery. The diet is limited to liquids for the first few days, and is advanced to a non-chew diet for the first four weeks. A soft-chew diet is then gradually advanced to a normal diet after six weeks of healing.
Though rare, if the teeth are wired together after surgery, a liquid diet would be required for six weeks after surgery. Typically one week off of work or school is required after surgery. Activity is restricted for the first four weeks with no lifting greater than 40 lbs. After four weeks, light activities can be resumed with low impact. Contact sports and rigorous activities can be resumed after 12 weeks or three months following surgery.
There are many ways to wire the teeth or jaws together. The term we use is maxillo-mandibular fixation or MMF for short. Though it is rare in conjunction with orthognathic surgery if required the orthodontic appliances or braces that the patient has on are used. Wires can be looped around the braces of the upper and lower teeth to wire the jaw shut.
The jaw may be wired shut due to trauma or mandibular fractures as well in order to immobilize it. It may also be wired for reconstructive purposes. This is typically done with either arch bars or Ivy loops.
An arch bar is a temporary brace that has hooks on it that can be secured to the teeth with wires. Once in place on the upper and lower teeth, the hooks are used to loop wires around that are used to wire the jaw shut.
Lastly, there are screw retained arch bars. This means that rather than securing the arch bar to the teeth with wires it is screwed into the bone of the maxilla and mandible. It too has hooks on it that can be used to loop wires around to wire the jaw shut.
The functionality of wiring the jaws or teeth together serves to immobilize the bones while they are healing, therefore acting like a cast. We ask patients who are wired together to carry wire cutters with them in case they are involved in an accident. It is usually not necessary for patients to cut their own wires.
With most orthognathic surgery or jaw surgery to move the maxilla and mandible, it is not necessary to wire the teeth together. Instead, we use titanium plates and screws as mentioned previously to secure the jaw into the new position. Occasionally, with very large movements or in the event of a less than ideal fracture the teeth or jaws may be wired together in order to immobilize the bones during the initial phase of healing. This is not very common.
The use of maxillo-mandibular fixation or MMF is not painful. The use of local anesthetics, conscious sedation, and occasionally general anesthesia make the process quite comfortable. After the completion of the procedure there can be some discomfort with the wires in the mouth, though this is usually very minor and can be managed with wax in sharp areas, the same as for traditional braces or orthodontic appliances.
When undergoing orthognathic surgery or corrective jaw surgery the majority of the incisions are hidden inside the mouth. The oral mucosa or gum tissue has an amazing capacity to heal and even intraoral scarring is minimal. Oftentimes, the application of the titanium screws in the mandible once in the new position, can require a small incision near the angle of the jaw. It is typically no larger than 2-4 mm and is usually not noticeable after three to six months.
If you are considering surgery for a severe misalignment of the teeth or jaws, first and foremost, you should visit an orthodontist. Correction of a malaligned, underdeveloped, or overdeveloped jaw requires a combined effort, usually including an orthodontist and an oral and maxillofacial surgeon.
Oral and maxillofacial surgeons have special training that requires extensive knowledge of facial surgery as well as dentistry, which makes them well equipped to manage surgery involving correction of a bad bite while also considering overall facial harmony. I would recommend relying on your orthodontist for ultimate referral though seeking care initially from an oral and maxillofacial surgeon is reasonable as well. The surgeon will likely provide a referral to a local orthodontist.
Following jaw surgery, we typically prescribe a mild analgesic in combination with a non-steroidal anti-inflammatory drug or NSAID like ibuprofen. With upper jaw surgery, we often give a nasal decongestant to decrease swelling of the nasal mucosa. In regards to antibiotics, an intravenous dose is provided pre-operatively and is continued post-operatively until discharge on a regular schedule. On discharge from the hospital your surgeon may recommend a short course of oral antibiotics.
A moderate amount of swelling is expected with orthognathic surgery. In order to limit the amount of swelling and improve patient comfort we utilize high-dose perioperative steroid administration. This includes an oral dose the evening prior to surgery followed by intravenous dosing in the operating room and post-operatively while in the hospital. The amount of swelling will vary from patient to patient. Typically after two weeks it is vastly improved and by four to six weeks it is 90 percent resolved. It may take up to six months for the last 10 percent of swelling to resolve, though this is typically only noticed by the patient and close family.
The incidence of infection following orthognathic or jaw surgery is very low. In the literature, the incidence is reported to be between 6 and 15 percent. These figures are high, in our opinion. When it occurs, the infection is easily treated with antibiotics and drainage with minimal discomfort and no long-term effects.
During jaw surgery, we utilize high-dose perioperative intravenous antibiotics for prophylaxis to prevent infection. Meticulous surgical technique and accomplishing the surgery in an efficient manner will also reduce infection rates. Occasionally, if bone grafts are utilized during surgery, we will continue the antibiotic therapy for seven to ten days orally after discharge. Our patients are also sent home with an antibacterial mouth rinse to help keep the wounds clean and are instructed on meticulous oral hygiene practices. Proper oral hygiene post-operatively is important in reducing the bacterial load in the mouth and adjacent to the surgical wounds.
Following an orthognathic surgery, we have patients return for numerous postoperative visits in order to ensure proper healing. We typically see patients at one week, four weeks, six weeks, and 12 weeks following surgery. We also see the patient back at the six-month and 12-month intervals once the orthodontic therapy is complete and the braces have been removed. A final set of records is obtained at that time. Close post-operative follow-up is important in order to catch any possible complications early as well as to ensure the proper bite and jaw position has been obtained and is stable.
JRA stands for juvenile rheumatoid arthritis. It is very different from the adult form. It is often a diagnosis of exclusion meaning all other diagnoses are ruled out. It can involve the temporomandibular joints. If so, management typically involves a team approach not only including the oral and maxillofacial surgeon and orthodontist, but rheumatologist and other physicians as well.
When it affects the temporomandibular joints JRA can lead to limited opening and malocclusion or a bad bite and misaligned jaws. It is often managed with newer medications typically guided by the rheumatologist. If the disease remains stable, then surgical correction of the bite can be undertaken by the surgeon and orthodontist with traditional orthognathic surgery. If the disease remains active and refractory to medical management, then total joint replacement of the temporomandibular joints may be necessary.
A cleft lip and/or palate is often associated with a cleft of the alveolus or the tooth bearing segments of the upper jaw or maxilla. The patient usually undergoes several surgeries in the area of the cleft at an early age. Because of this early surgery, the normal growth pattern of the maxilla can be restricted.
It is often necessary to advance the upper jaw when the patient is in the mid to late teens. This can be completed in a single surgery and may also be combined with a lower jaw or mandibular surgery. At times, if the movement is too large to complete in a single surgery, a procedure called distraction osteogenesis may be undertaken to reposition the jaw. This procedure grows the jaw over a period of weeks to achieve the desired position. It is typically reserved for very large discrepancies.
Distraction osteogenesis of the jaws is based on the Ilizarov leg lengthening procedure. In many ways, it is more successful and reliable in the head and neck region versus the extremities because of the ample blood supply found in the head and neck. It is typically reserved for very severe deformities that cannot be corrected in a single surgery.
In the mandible or lower jaw it is at times used to advance and grow the jaw forward in order to open the airway and avoid the need for tracheostomy in infants and children with severe micrognathia (small mandible).
As mentioned previously in the maxilla or upper jaw it is often times used in patients who have undergone cleft lip and palate repairs, which can restrict maxillary growth. This can lead to a more severe misalignment of the jaws. Distraction osteogenesis can be utilized in these cases to grow the jaw over a period of time to correct a more severe discrepancy.
The distraction osteogenesis procedure can take more time than traditional orthognathic surgery. During an initial surgery, devices are placed on the mandible or the maxilla. These devices are then turned twice a day by the patient at home, or in the case of infants by the surgeon in the hospital. This advances or grows the jaw by 1 mm per day. A typical advancement may range from 10-15 mm. That would require up to two weeks of turning. Once the growth is complete the devices are no longer turned and remain in place for about 6-12 weeks to allow the new bone to calcify and heal. After this period a second surgery is undertaken to remove the implanted devices.
Following orthognathic surgery, there will be neurosensory changes. The nerves involved with jaw surgery are not motor, meaning surgery will not affect how your face looks or moves. In the lower jaw, the numbness will include the lower lip, chin, and gum tissue, and in general, this should resolve in about three months. Sometimes neurosensory changes take up to 18 months in an adult to resolve completely.
Occasionally, minor neurosensory changes of the lower lip and chin can be permanent. Permanent numbness following an upper jaw (maxilla) surgery is much less common.
Dental disease is a very common problem in both young and old cats. It is thought that as many as 85% of cats aged three years and older have some sort of dental disease.
Dental disease tends to be more common and be more severe as cats get older, just as in humans. Dental disease in cats is commonly associated with the accumulation of dental plaque (as a result of bacteria in the mouth) and tartar formation, this can result in what is termed ‘periodontal disease’ – disease affecting the teeth and the structures around the teeth that support and keep them healthy.
Plaque is a complex film of bacteria that develops on the surface of teeth. Initially, the plaque layer is not readily visible, but it can be demonstrated by using a ‘disclosing solution’ that stains the plaque film. As the plaque layer grows and becomes thicker, it can often be seen as a soft, grey or white film on the tooth surface.
Plaque is important because it is the most common underlying cause of dental disease. Taking measures to help reduce dental plaque development is, therefore, an important step in trying to prevent dental disease in cats. Plaque can be removed with brushing helping to keep the gums healthy.
If plaque is left undisturbed it can become hardened due to deposition of substances such as calcium in the plaque layer. Hard, calcified plaque is known as dental ‘tartar’ or ‘calculus’.
Tartar is clearly visible and looks like a cream/yellow or brown hard deposit on the tooth surface. In severe cases, a large amount of tartar can develop on the surface of the tooth. Tartar, because it is so hard, cannot usually be removed by simple measures such as brushing the teeth, and dental scaling (performed by your vet under an anaesthetic) is usually required to remove it.
Dental disease can affect cats of any age and varies in severity – some cats develop severe disease at a relatively young age. Several factors affect the development of disease including:
Teeth that are positioned abnormally in the mouth (malaligned) are more likely to accumulate plaque and tartar than those which are correctly positioned. This is because when malaligned, the teeth are not cleaned by the natural abrasion that occurs when food is eaten and chewed. Reasons for misalignment include:
Breed – Very short-nosed breeds or variants in breeds (eg, Persians, Chinchillas, British and Exotic Shorthairs) almost invariably have abnormally positioned teeth, sometimes severely so. Their jawbones are often too small to accommodate the teeth, resulting in overcrowding and misalignment of teeth.
Deciduous tooth retention – In some cats, deciduous teeth (‘baby teeth’ or ‘milk teeth’) can be retained after the permanent teeth have erupted (grown through). If the adult tooth does not push the deciduous tooth out when it erupts, the adult tooth may grow at an abnormal angle, resulting in permanent misalignment.
Trauma or congenital abnormalities – Sometimes the jaw of a cat may have an abnormal shape either because the cat has a congenital abnormality (an abnormality present from birth, such as an undershot or overshot jaw), or perhaps as a result of trauma (eg, a healed, fractured jaw). These can also cause tooth misalignment.
Diet is thought to play a role in the progression of some cats with dental disease. It is possible that feeding only soft/wet food provides little or no abrasive action against the teeth when chewing, and so offers little to prevent plaque formation. Indeed the food itself may accumulate on or around the teeth and encourage bacteria and plaque formation. Dry foods tend to encourage chewing and tend to be more abrasive but the relationship between food and dental disease is complex and the structure of the solid chunks of food is probably more important than whether the food is wet (tinned or sachet) or dry.
Some special diets are available from your vet that are specifically aimed to help prevent plaque and tartar formation. These diets are designed with kibble/biscuit or with special chunks in the wet food that increase tooth penetration and provide a more abrasive action against the tooth to reduce tartar accumulation.
Some infectious diseases are associated with gingivitis and your vet may advise screening for feline immunodeficiency virus (FIV) infection and feline leukaemia virus (FeLV) infection, or feline calicivirus (FCV). FIV and FeLV can cause immunosuppression and may predispose to periodontal disease and gingivitis, whereas persistent FCV in the mouth may also be associated with some cases of chronic (long-standing) gingivitis or stomatitis (inflammation of the gums or mouth).
Cats should ideally have their teeth examined by a vet at least once every 12 months, and cats that have had dental problems should be examined once every 3-6 months depending on their condition. Generally, the sooner the problem is identified, the easier and quicker it is to treat. Even if the cat’s mouth is being examined every day, dental disease will develop and gradually progress. Cats will quite often not show clinical signs until the disease is advanced by which time many teeth may need to be extracted.
Mild gingivitis – is very common in cats of all ages. It can occur as quickly as 48 hours after cleaning when plaque formation may have begun. Mild gingivitis does not affect the tooth root and home care of the teeth and may easily reverse most cases.
Moderate gingivitis – is also very common. If plaque accumulates on the teeth, the gingiva will become more inflamed as time progresses. Sometimes gum recession can be seen at this stage. Gingival “pockets” may also be evident, which is where the gum has started to separate from the tooth, providing a perfect site for food, bacteria, plaque and tartar to accumulate. If calculus hasn’t already formed, many cases of moderate gingivitis may also be reversed with regular daily home care. However, gingival pocket formation is difficult to reverse.
Severe gingivitis – can be very painful for a cat. The cat may show signs of hypersalivation (drooling), halitosis, pawing at the mouth, difficulty eating and sometimes bleeding from the mouth. Severe gingivitis is common in cats that have a lot of plaque and calculus on their teeth. Gum recession is also common, but may not always be obvious since the gums are so inflamed. Gingival pockets can be seen and are usually deeper than those found with moderate gingivitis. Severe gingivitis cannot usually be reversed with brushing, and often the mouths are too sore to brush. The cat will usually require a general anaesthetic to carry out a scale and polish of the teeth. If there is a severe degree of gum recession exposing the tooth root then the tooth may need to be extracted. Regular brushing is strongly advised afterwards to prevent the disease from recurring.
Cats of around five months of age quite commonly develop gingivitis and you may notice an obvious smell to your cat’s breath. This is usually due to permanent teeth erupting through the gums and loss of deciduous teeth causing gum disturbance and inflammation. You may even find a tooth lying on the floor at home! This is completely normal and will normally take 4-6 weeks to settle down. However, if the cat is showing any signs of discomfort then it should be examined by a vet.
Periodontitis is gum disease that is very advanced and more commonly found in older cats. The gums are usually very inflamed and often recessed. Large amounts of calculus are usually present on the teeth. The ligaments surrounding and supporting the tooth are also diseased and have usually begun to break down exposing the tooth root and causing the tooth to be very unstable. Bacterial infection is common and often pus can be seen surrounding the tooth. Clinical signs are similar to those of severe gingivitis. At this stage, the tooth is so diseased that extraction is the only treatment option.
Stomatitis means inflammation of the oral cavity (inside the mouth). Cats can suffer from a condition known as lymphocytic plasmacytic gingivostomatitis complex (LPGC) or chronic gingivostomatitis. In this disease, inflammation spreads from just the ginigiva to other areas of the mouth as well. This most often happens to the back of the mouth (the area called the ‘faces’ or the ‘glossopalatine folds’), however, the inflammation can extend virtually anywhere in the mouth.
The exact cause of this disease is still unknown. Some cases are associated with persistent FCV infection, and FIV infection may predispose to this. However, while dental plaque and some calculus may be present, the amount of inflammation is quite disproportionate and it is thought that some immune dysregulation is involved in the disease where the cat’s immune system may be responding too aggressively to the presence of bacteria or other infectious agents in the mouth.
This is an extremely painful disease and cats will often have difficulty eating, hypersalivate (drool), paw at the mouth and show other signs of mouth pain. They may lose weight with the reduced appetite.
Various treatments may be used including initial scaling and cleaning of the teeth, follow-up home care, antibiotics and anti-inflammatories. The response to therapy is variable and many cats need corticosteroids to control the inflammation and sometimes other more potent anti-inflammatory or immunosuppressive drugs. In some very severely affected cats, extraction of all of the cheek teeth is helpful – this may be because it removes the site of persistent bacteria in the mouth.
Feline resorptive lesions (FRLs) are common in both young and old cats. It has been estimated that more than 70% of cats over five years have at least one FRL.
A FRL is an erosion in the tooth, commonly formed around the gum line (the neck of the tooth) but can also be found below the gum line in some cats. The cause of FRLs is unknown but cells called odontoclasts (which break down the substance of the tooth) are found in the erosions.
When examining a cat’s mouth a FRL can be difficult to identify (and your vet will often need to probe the teeth under an anaesthetic to identify them), but they appear as a small amount of gum growing out of the tooth. In fact, the gum is inflamed due to the cavity and reacts by ‘filling in’ the hole in the tooth.
FRLs can be diagnosed by dental X-rays or by probing the teeth under general anaesthesia. FRLs are extremely sensitive, and cats will often exhibit signs of pain associated with them. If FRLs are left they cause gradual erosion of the tooth to the point where the crown will fracture off leaving the root behind. The cavities produced by FRLs are not due to decay like human and canine dental cavities, therefore filling them is unsuccessful and affected teeth need to be removed.
Fractured teeth need to be assessed individually before deciding if extraction is necessary. As a general rule, teeth that have fractured through to the dentine or pulp cavity (affecting the nerve and blood supply) are likely to need extraction as the tooth will be painful and it will be at risk of developing an infection and tooth root abscess. If only the tip of a crown is fractured, and the dentine or pulp cavity are not exposed then the tooth may not need to be extracted. However, the enamel covering a cats tooth is so thin that the majority of fractured teeth will almost certainly have to be removed. A probe can be used to assess if the tooth needs extracting. Signs such as pawing at the mouth, hypersalivation and favouring one side of the mouth when eating may be seen in cats with a fractured tooth.
Understandably animals will not sit still and allow dental work to be done, so this should always be carried out under a general anaesthetic. However, dental disease can be easy to overlook, or even ignored. Although anaesthetising a cat can be worrying, the longer the teeth are left, the longer the anaesthetic and procedure will take because dental disease will have progressed. Measures can be taken to reduce the risk of an anaesthetic such as blood tests, and in older cats, intravenous fluid therapy can be given to help support the circulation throughout the anaesthetic. If you are worried about your cat undergoing an anaesthetic then you should discuss your concerns with your vet.
All our advice is freely accessible to everyone, wherever you are in the world. However, as a charity, we need your support to enable us to keep delivering high quality and up to date information for everyone. Please consider making a contribution, big or small, to keep our content free, accurate and relevant.

Many people may have a prognathic face from birth, and it may not be a problem. Prognathism can cause complications that may require treatment, such as misaligned teeth.
If you have prognathism that’s caused by an underlying medical condition, such as gigantism or acromegaly, you may also need additional treatment for that condition.
Gigantism is an increase in growth hormone before the growth plates in the bones have closed, and the condition presents in kids. Acromegaly is also an increase in growth hormone, but the increase occurs after the growth plates have closed, and the condition presents in adults.
Basal cell nevus syndrome, or Gorlin syndrome, affects an estimated 1 in 31,000 people. Basal cell nevus syndrome raises your risk for a type of skin cancer called basal cell carcinoma.
If you develop unusual spots or growths on your skin, let your healthcare provider know. If they suspect that the spot or growth might be cancerous, they may refer you to a dermatologist for testing.
Markings in the shape of a saddle over the back. Color definitions may vary by breed. Always check the breed standard for the definitive color description.
Used to describe several breeds, this color is a dull, yellowish gray of medium saturation. Color definitions may vary by breed. Always check the breed standard for the definitive color description.
Used to describe Boston Terriers, this color appears black except that it has a red cast when viewed in the sun or bright light. Color definitions may vary by breed. Always check the breed standard for the definitive color description.
A division of the regular or primary class. The division can be breed-specific, having to do with color, height, weight, or coat (e.g., Open-Fawn), or event-specific (e.g., Novice A or B in obedience events). Best of Breed or Best of Variety are not divided into secondary classes. Secondary classes are offered at the discretion of the Event Committee of the club holding the event.
Used to describe Chesapeake Bay Retrievers, this color is similar to deadgrass, but it is more accurately a lightening of the chocolate hue. Color definitions may vary by breed. Always check the breed standard for the definitive color description.
One color or whole color except for lighter shadings. Color definitions may vary by breed. Always check the breed standard for the definitive color description.
A suffix title conferred on dogs that have qualified the required number of times in Senior tests at hunting tests for pointing breeds, retrievers, and spaniels.
A prefix title conferred on dogs that have earned the Grand Nite Champion and have won the required number of first placements in AKC Coonhound night hunts.
All footprints falling on a single line of travel. When a dog breaks into a trot, his body is supported by only two legs at a time, which move as alternating diagonal pairs. To achieve balance, his legs angle inward toward a center line beneath his body, and the greater the speed, the closer they come to tracking on a single line.
A gait fault indicated by a quick outward snatching of the hock as it passes the supporting leg and twists the rear pastern far in beneath the body. The action causes noticeable rocking in the rear quarters.
The state of mental and physical health when all organs and faculties are complete and functioning normally, each in its rightful relation to the other.
An event or class, restricted to purebred dogs, that is not normally offered at an AKC all-breed or specialty event. Special permission may be granted to open the event to breeds not recognized by the AKC or to a well-known dog with a celebrity. Examples of Special attractions are:
A department that specializes in handling anything outside the normal domestic registration; e.g., Foreign Applications, Open Registry, and Special Litters.
Department formed at the AKC to handle questions and problems that come from the show group of customers of the AKC. Designed to offer a premium level of service to those significantly involved in the sport.
Deep red (almost brown) with intermingling of black hairs (Miniature Pinscher). Color definitions may vary by breed. Always check the breed standard for the definitive color description.
Person who is responsible for the smooth running of a specific ring; for example, assembling the classes, distributing armbands, etc., thereby enabling the judge to concentrate on judging the dogs.
Monthly publication of the AKC. A listing of dogs that have sired or produced a litter that has been registered with the AKC. With this information, a person can use Stud Book volumes to trace a dog’s lineage and to produce pedigrees.
Class where a stud dog is shown and judged with at least two of his offspring. Judging is based on the quality of the get, not the sire. (Club may permit more offspring to be shown. The upper limit must be stated in the Premium List.)
A completed form (used primarily by handlers) that authorizes the AKC to accept the signature of someone other than the actual owner of the stud dog named. This form can be used only on litter applications for litters sired by that dog. The form is valid for one year; a new form must be filed to extend authorization.
The form that must be completed by the current owner and the new owner when a registered or registerable dog changes hands more than once before being transferred or registered. This form is attached to the original registration certificate or application. Also called the gray form.
A non-regular competition offered in conjunction with regular classes at specialty shows for puppies or veterans. Class divisions, requirements, and conditions are established by the club. No championship points are awarded.

To achieve strong oral health and a wonderful smile, your upper and lower jaws need to evenly meet. This allows you to do things like eating and swallowing with ease and avoid some very serious health risks to your jaw, mouth and teeth.
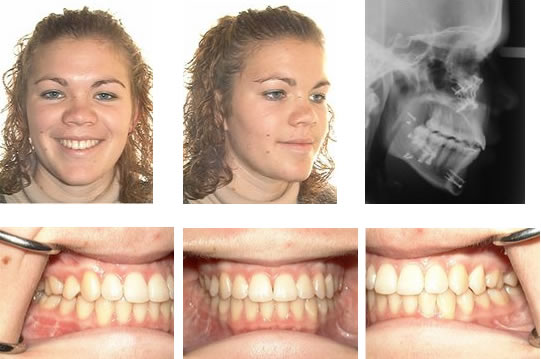
A malocclusion is whenever the upper and lower rows of teeth do not meet. There are three types of malocclusions: overbites, underbites and crossbites. Overbites and underbites are the most common but all three require immediate and thorough orthodontic treatment. It can be tricky to know if you have a severe enough overbite or underbite to warrant orthodontic intervention.
How do you go about fixing your overbite or underbite? How do the treatments differ? What can you expect from the various treatments? As you can imagine, there are a lot of questions that you need answered. To start, let’s review the basics of identifying overbites and underbites. Then, we’ll explore treatment options and the best courses of action with respect to dealing with your malocclusion before the problem worsens.
Just because your upper teeth extend somewhat over your lower teeth, doesn’t necessarily mean you have an overbite. In addition, minor overbites are very common and might not require braces. Overbites that are severe enough to need fixing occur when the upper teeth overlap the bottom teeth to an excessive degree of roughly 4 to 10 millimeters. This can be caused by genetics, a recessive chin, misaligned bites, thumb sucking, poorly fitted crowns, gum disease or as the result of injury. Also, sometimes teeth just come in awkwardly.
Overbites are more common than underbites and are called a Class II bite. One thing to remember is that having a slight overbite is normal because the shape of the human skull naturally allows for the upper teeth to extend beyond the lower teeth. During checkups, your dentist should measure your overbite and underbite and consult with you if they suspect any issues.
The good news is that overbites are considered to be easily treatable using conventional methods. It is easier to fix in young children so don’t hesitate to speak with an orthodontist immediately about your child or children’s potential malocclusion. It’s never too late to fix this issue if the patient is willing.
An underbite, a Class III bite, is when the lower teeth extend beyond the upper. Essentially, the lower jaw protrudes, making it impossible for the lower row of teeth to align with the upper row causing the potential for several serious oral health issues. This can be caused by the upper jaw bone being underdeveloped or the bone in the lower jaw being overdeveloped.
Like overbites, underbites can begin during childhood due to behaviours like thumb-sucking or caused by genetics or as the result of an accident. Whatever the cause, severe underbites should be treated immediately as to avoid the potential hazards that can surface over time.
Most people believe there are only two malocclusions. There is a third type, though, known as a crossbite. And while it is less common, it still requires diagnosis and treatment. Crossbite is a lateral misalignment meaning the top teeth are positioned too close to the cheek or tongue.
Crossbite occurs during childhood and doesn’t naturally correct itself over time. It can occur between the front or back teeth. The side effects are similar to and just as serious as overbites and underbites. Upon diagnosis, your dentist should present treatment options and recommend a course of action.
While you can do a remedial check to see if you exhibit the signs of having a misaligned bite, this is a job best left to your dentist or orthodontist. They will conduct an inspection that looks for:
There are also mental health and self-esteem risks associated with overbites and underbites. This is often overlooked but our appearance can inform how we feel and determine our emotional state. We believe that dentistry should help you feel confident and comfortable with your smile.
For less severe bites, a removable retainer is a suitable enough solution to produce the desired results. This type of retainer hooks around the back teeth to hold itself securely in place. The removable element makes it easier to clean your teeth but the patient must be responsible enough to remember to put it in every day. Forgetting for long stretches would negate this treatment’s effectiveness.
The most common way to treat misaligned bites is with braces or aligners, especially with children or teenagers. Braces use taut wires to connect tiny brackets to apply consistent pressure to teeth. This forces them to realign and straighten over time. Braces have a high success rate but can be pricy and patients must wear them for anywhere between one to three years.
If you need more incentive to deal with a misaligned bite early, keep in mind that insurance providers often cover braces for children but not adults. We always recommend speaking with your insurance provider to discuss your coverage and payment options.
Some cases of misaligned bites only require aligners. Popular options like Invisalign, which are clear and removable, work wonders while allowing people to go about their day with minimal interruption or embarrassment. Invisalign isn’t an appropriate solution for every case of malocclusion so ask your dentist if they make sense for your situation.
Treatment duration depends on the severity of your issue but be prepared to commit for several months if not a year or two. It might sound as if treatment will upend your life but it is worth it for both your oral health and the smile you will achieve and get to show off every day. Your dentist should be well equipped to talk you through the emotional impact of these procedures and help prepare you for any changes to your daily life.
Don’t wait and let your overbite, underbite or crossbite worsen and create additional issues for your mouth, teeth and gums. Letting these problems linger can result in you needing caps, crowns or dental hardware installed. Furthermore, neglect can make them harder to fix down the road.
We hope this article has answered some of your questions about overbites and underbites. If you or your child needs treatment, then remember just about any misaligned bite can be repaired. It’s always better to tackle the problem head-on and immediately.

Enzo is the Hawthorne Hills Veterinary Hospital Pet of the Month for May. Everyone knows that puppies need vaccines to keep them healthy and protected from diseases. However, it can be easy to underestimate the benefits of thorough and regular examinations when puppies are growing into adulthood. Every breed has special characteristics that make them unique and add to their appeal and sometimes there are physical changes that need to be addressed quickly. For this reason our veterinarians believe in examinations with every vaccine, especially during a puppy’s formative months.
Enzo is a short-haired Havanese and he was born with his lower jaw shorter than the upper jaw. This is called an Overbite, also referred to as an Overshot Jaw, a Parrot Mouth or Mandibular Brachygnathism. This malocclusion is a genetic change and can be seen in a number of breeds, oftentimes collie related breeds and dachshunds. Occasionally this change happens because of differences in the growth of the upper and lower jaws, and in many cases it doesn’t cause any significant problems other than cosmetically.
Dr. Robin Riedinger evaluated Enzo at his first visit when he was just 11 weeks of age and while the lower jaw was too short, there was no evidence of damage and no indication that this was causing a problem for Enzo. When there is abnormal occlusion of the teeth, it is important to monitor closely for trouble caused by the teeth being aligned improperly. Malocclusions can lead to gum injuries, puncturing of the hard palate, abnormal positioning of adjacent teeth, abnormal wear and bruising of the teeth, permanent damage and subsequent death of one or more teeth, and in the long run, premature loss of teeth. Some malocclusions can be severe enough to interfere with normal eating and drinking.
Within three weeks, when Enzo was only 3.5 months old, it was clear that our doctors would need to intervene. The left and right sides of Enzo’s upper jaw (maxilla) were growing at different rates because the lower canine teeth were being trapped by the upper canine teeth. This is called Dental Interlock. Because the teeth are ‘locked’ in place, the lower jaw cannot grow symmetrically and this creates a number of other problems. Early intervention is critical.
The solution for Dental Interlock is to extract the teeth from the shorter jaw; in this case, the lower ‘baby’ canines and thereby allow the lower jaw (mandible) to grow in the best way possible. This procedure is most effective when the Dental Interlock is discovered early and the extractions are performed quickly. In some cases, this can be as early as ten weeks of age. Dr. Riedinger consulted with a local veterinary dental specialist to confirm the treatment plan and to get advice on extracting the deciduous teeth without damaging the developing adult canines. Dental radiographs are essential to proper extraction technique and also to ensure that there are no other abnormalities below the gumline.
You can see how long the roots of the deciduous ‘baby’ teeth are. During normal growth, the body will begin to resorb the roots, making them loose, and allow them to fall out as the adult tooth begins to emerge. When we need to remove the deciduous teeth before they are loose, it can be quite tricky to remove the tooth carefully without breaking it and without injuring the adjacent teeth.
Once extracted, each deciduous canine tooth was about 2 centimeters long; the roots were about 1.5 centimeters. Many people are surprised to learn that the root of a dog’s tooth is so large – 2/3 to 3/4 of the tooth is below the gumline. This is one reason why it is so important to use radiographs to evaluate teeth on a regular basis, not just in a growing puppy. Adult teeth can, and frequently do, have problems that are only visible with a radiograph.
Enzo came through his procedure extremely well. He was given pain medications for comfort and had to eat canned foods and avoid chewing on his toys for the next two weeks to ensure that the gum tissue healed properly. As he continues to grow we will be monitoring how his jaw develops and Dr. Riedinger will also be watching the alignment of his adult canine teeth when they start to emerge around six months of age. Hopefully this early intervention will minimize problems for Enzo in the future.
Joining the chorus of voices condemning the Trump administration"s ongoing trade war with China, the American Fly Fishing Trade Association (AFFTA) recently released a statement denouncing the administration"s decisions as "unfair" and "harmful" to the $1 billion fly fishing industry, an industry whose backbone, AFTTA says, is small and medium-sized businesses.
The statement, from AFFTA CEO Ben Bulis, also chided the Trump administration for handing off the costs of tariffs to anglers. Though Trump regularly and falsely makes public proclamations indicating that China is paying U.S.-levied tariffs, economists and policy makers have repeatedly tried to set the record straight by explaining that tariffs on goods and materials imported from China are paid by the U.S. companies that import those goods, which then pass those costs onto the U.S. consumer in the form of higher prices.
Bulis wrote, "From specialty retail shops, guides and outfitters to the manufacturers who develop and produce the gear that they rely on for their livelihood, we are a significant part of our nation’s powerful and growing outdoor economy, contributing more than $1 billion annually. This increase in tariffs, on top of the already harmful tariffs imposed over the past 10 months, will only make it more difficult and costly for our industry’s businesses and the local economies that rely on them to stay viable. The increase will further stifle innovation, force unfair and highly expensive production changes, inhibit the free market and freeze, or worse, cut employment ... Even further, this increase will saddle American consumers, including ove




 8613371530291
8613371530291