overshot jaw in puppies price

This website is using a security service to protect itself from online attacks. The action you just performed triggered the security solution. There are several actions that could trigger this block including submitting a certain word or phrase, a SQL command or malformed data.
Enzo is the Hawthorne Hills Veterinary Hospital Pet of the Month for May. Everyone knows that puppies need vaccines to keep them healthy and protected from diseases. However, it can be easy to underestimate the benefits of thorough and regular examinations when puppies are growing into adulthood. Every breed has special characteristics that make them unique and add to their appeal and sometimes there are physical changes that need to be addressed quickly. For this reason our veterinarians believe in examinations with every vaccine, especially during a puppy’s formative months.
Enzo is a short-haired Havanese and he was born with his lower jaw shorter than the upper jaw. This is called an Overbite, also referred to as an Overshot Jaw, a Parrot Mouth or Mandibular Brachygnathism. This malocclusion is a genetic change and can be seen in a number of breeds, oftentimes collie related breeds and dachshunds. Occasionally this change happens because of differences in the growth of the upper and lower jaws, and in many cases it doesn’t cause any significant problems other than cosmetically.
Dr. Robin Riedinger evaluated Enzo at his first visit when he was just 11 weeks of age and while the lower jaw was too short, there was no evidence of damage and no indication that this was causing a problem for Enzo. When there is abnormal occlusion of the teeth, it is important to monitor closely for trouble caused by the teeth being aligned improperly. Malocclusions can lead to gum injuries, puncturing of the hard palate, abnormal positioning of adjacent teeth, abnormal wear and bruising of the teeth, permanent damage and subsequent death of one or more teeth, and in the long run, premature loss of teeth. Some malocclusions can be severe enough to interfere with normal eating and drinking.
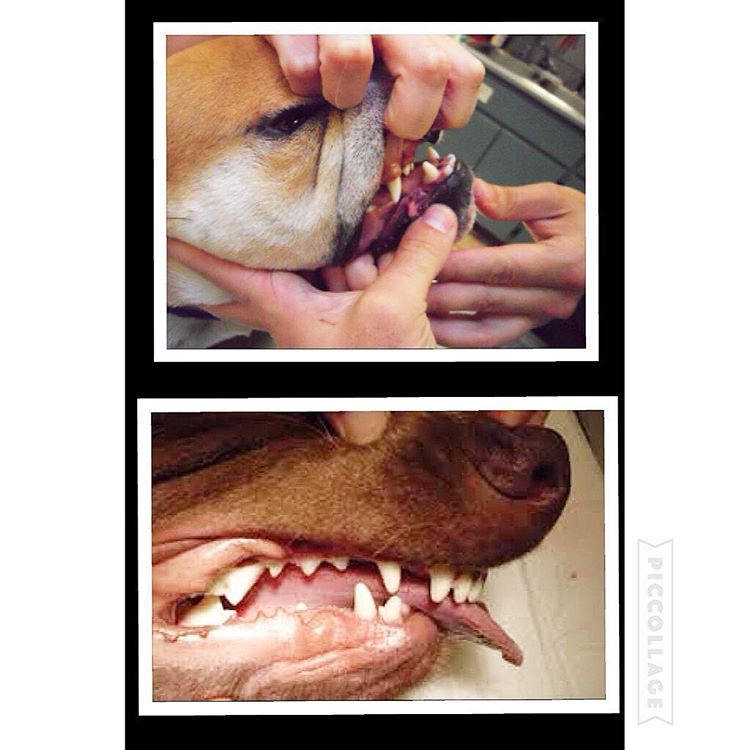
Within three weeks, when Enzo was only 3.5 months old, it was clear that our doctors would need to intervene. The left and right sides of Enzo’s upper jaw (maxilla) were growing at different rates because the lower canine teeth were being trapped by the upper canine teeth. This is called Dental Interlock. Because the teeth are ‘locked’ in place, the lower jaw cannot grow symmetrically and this creates a number of other problems. Early intervention is critical.
The solution for Dental Interlock is to extract the teeth from the shorter jaw; in this case, the lower ‘baby’ canines and thereby allow the lower jaw (mandible) to grow in the best way possible. This procedure is most effective when the Dental Interlock is discovered early and the extractions are performed quickly. In some cases, this can be as early as ten weeks of age. Dr. Riedinger consulted with a local veterinary dental specialist to confirm the treatment plan and to get advice on extracting the deciduous teeth without damaging the developing adult canines. Dental radiographs are essential to proper extraction technique and also to ensure that there are no other abnormalities below the gumline.
You can see how long the roots of the deciduous ‘baby’ teeth are. During normal growth, the body will begin to resorb the roots, making them loose, and allow them to fall out as the adult tooth begins to emerge. When we need to remove the deciduous teeth before they are loose, it can be quite tricky to remove the tooth carefully without breaking it and without injuring the adjacent teeth.
Once extracted, each deciduous canine tooth was about 2 centimeters long; the roots were about 1.5 centimeters. Many people are surprised to learn that the root of a dog’s tooth is so large – 2/3 to 3/4 of the tooth is below the gumline. This is one reason why it is so important to use radiographs to evaluate teeth on a regular basis, not just in a growing puppy. Adult teeth can, and frequently do, have problems that are only visible with a radiograph.
Enzo came through his procedure extremely well. He was given pain medications for comfort and had to eat canned foods and avoid chewing on his toys for the next two weeks to ensure that the gum tissue healed properly. As he continues to grow we will be monitoring how his jaw develops and Dr. Riedinger will also be watching the alignment of his adult canine teeth when they start to emerge around six months of age. Hopefully this early intervention will minimize problems for Enzo in the future.

An overbite might not seem like a serious condition for your dog, but severely misaligned teeth can lead to difficulty eating, gum injuries and bruising, bad breath and different types of dental problems, including tooth decay and gingivitis. Fortunately, there are ways to help fix the problem before it becomes irreversible.
An overbite is a genetic, hereditary condition where a dog"s lower jaw is significantly shorter than its upper jaw. This can also be called an overshot jaw, overjet, parrot mouth, class 2 malocclusion or mandibular brachynathism, but the result is the same – the dog"s teeth aren"t aligning properly. In time, the teeth can become improperly locked together as the dog bites, creating even more severe crookedness as the jaw cannot grow appropriately.
This problem is especially common in breeds with narrow, pointed muzzles, such as collies, shelties, dachshunds, German shepherds, Russian wolfhounds and any crossbred dogs that include these ancestries.
Dental examinations for puppies are the first step toward minimizing the discomfort and effects of an overbite. Puppies can begin to show signs of an overbite as early as 8-12 weeks old, and by the time a puppy is 10 months old, its jaw alignment will be permanently set and any overbite treatment will be much more challenging. This is a relatively narrow window to detect and correct overbites, but it is not impossible.
Small overbites often correct themselves as the puppy matures, and brushing the dog"s teeth regularly to prevent buildup can help keep the overbite from becoming more severe. If the dog is showing signs of an overbite, it is best to avoid any tug-of-war games that can put additional strain and stress on the jaw and could exacerbate the deformation.
If an overbite is more severe, dental intervention may be necessary to correct the misalignment. While this is not necessary for cosmetic reasons – a small overbite may look unsightly, but does not affect the dog and invasive corrective procedures would be more stressful than beneficial – in severe cases, a veterinarian may recommend intervention. There are spacers, braces and other orthodontic accessories that can be applied to a dog"s teeth to help correct an overbite. Because dogs" mouths grow more quickly than humans, these accessories may only be needed for a few weeks or months, though in extreme cases they may be necessary for up to two years.
If the dog is young enough, however, tooth extraction is generally preferred to correct an overbite. Puppies have baby teeth, and if those teeth are misaligned, removing them can loosen the jaw and provide space for it to grow properly and realign itself before the adult teeth come in. Proper extraction will not harm those adult teeth, but the puppy"s mouth will be tender after the procedure and because they will have fewer teeth for several weeks or months until their adult teeth have emerged, some dietary changes and softer foods may be necessary.
An overbite might be disconcerting for both you and your dog, but with proper care and treatment, it can be minimized or completely corrected and your dog"s dental health will be preserved.

Malocclusion in dogs causes an abnormal alignment of the teeth, which results in an abnormal bite. A dog whose lower jaw is protruding and with the bottom teeth sticking out when at rest is known as an underbite dog.
We will focus on “class 3 malocclusions,” also known as an underbite. This condition happens when the lower jaw teeth protrude forward relative to the upper jaw teeth.
Class 1 malocclusion, on the other hand, occurs when the upper and lower jaws are proportionally in shape in length, but the teeth don’t come together properly.
Dental is probably the number one cause of malocclusion in dogs. Dental underbites occur when one or a couple of teeth are abnormally positioned within a normal facial skeletal structure, says Dr. Santiago Peralta, assistant professor of veterinary dentistry and oral surgery at Cornell University College of Veterinary Medicine (CUCVM).1
Dental underbite commonly happens when a baby tooth fails to fall out and is still present when a permanent tooth erupts. This causes crowding among teeth. Thus the abnormal position and underbite look in your dog.
This cause of underbite on dogs is the easiest to correct. According to Sacramento Veterinary Dental Services, the extraction of the primary teeth (interceptive orthodontics) should be performed as soon as possible to correct the problem.2
Dr. Nadine Fiani, assistant clinical professor of dentistry and oral surgery at CUCVM, says the skeletal type of malocclusion is where the dog’s facial structure is abnormal, causing the teeth not to fit together correctly.
Skeletal underbite in dogs may be more problematic than dental.An abnormal mouth bone structure may cause the canine teeth or maxillary incisors to make abnormal contact with the gums causing severe distress and damage to your pup’s teeth and gums. This could fasten the rapid onset of periodontal disease.
“[A dog underbite] will be acquired, whether because something happened during gestation or something happened during growth and development. The condition can develop due to an infection, trauma, or any other event that may alter maxillofacial [face and jaw] growth.”
A dog underbite may also be caused by jaw fractures that don’t heal properly. Trauma to the face and jaw caused by bites, accidents, or getting hit by a car can cause your dog to develop an underbite.
Fortunately, most dog underbites do not require any treatment. If the underbite is not causing damage to a dog’s mouth (i.e., preventing chewing or swallowing), there may be no need for treatment.
2. Crown modification is often used for shortening or modifying crowns to prevent the tooth from causing trauma and using orthodontics to move the tooth into the correct position.
Any dog breed can develop an underbite. However, Class 3 malocclusions (dog underbite) are more common in brachiocephalic dog breeds, like Pugs and Bulldogs. However, an underbite can appear in any dog breed.
Most malocclusions are genetic. It’s important to have your dog’s bite evaluated for non-symmetrical jaw growth by a professional, especially if your dog is brachycephalic.
Upon examination, your vet should recommend treatment if necessary. In some cases, underbites don’t cause any irritation and are nothing to worry about. Be sure to request a dental radiograph (X-rays) for your pet. This will help identify most oral diseases in dogs.
Orthodontic treatments for dogs with underbites vary in price depending on the condition, the number of teeth involved, rounds of anesthesia, among other factors. The treatment cost of malocclusion in dogs usually fluctuates between $1,500 and $4,000, according to PetMD.
Underbite in puppies may sometimes be corrected using braces. However, extraction and filling can also be applied. Treatment options for a puppy with underbites will vary depending on the type of malocclusion your pet faces, age, health status, and other factors.
Just like adult dogs, puppies with underbites are prone to health issues. If your dog has an underbite, seek medical attention to determine if your puppy’s underbite is detrimental to his health.
An underbite is permanent and generally does not get worse with age. Dogs with underbites do not have many problems. However, the main issue you may encounter is that the teeth align and rub against each other and create a wound within the gums or hard palate.
Switching from hard to soft dog food is advised when living with a dog with an underbite. Some dogs with underbites tend to have trouble chewing their food. Nom Nom fresh dog food is a great alternative to aid when this happens and to put less stress on your dog’s teeth when eating his food.
When it comes to dog treats for dogs with underbites, consider these soft-baked dog treats by Merrick or American Journey’s soft chewy dog treat. You also want to provide a soft chewing dog toy like Chuckit! Roller Dog Toy. Its textured chenille fabric is gentle on dogs’ mouths.
Dogs whose teeth have been extracted or re-shaped must maintain a strict recovery period by only eating soft foods. Regular cleaning is needed to make sure the dog’s teeth continue to be healthy. Be sure to brush your dog’s teeth regularly.
We love using our Dental Kit from Bark Bright. This veterinarian formulated enzymatic toothpaste has three enzymes that break down the debris that cause bad breath.
This helps promote fresher breath and cleaner mouth reducing the chances of periodontal disease, which is more common in dogs with underbites and present in 80% of dogs have by age 3. No toothbrush required.
Finally, dogs with underbites often develop excessive tartar and calculus build-up. Hence, it’s also a good idea to target the build-up of plaque and tartar with a Dental Formula Water to leave your dog’s teeth and gums in tip-top condition.
A dog’s bite typically sets at ten months old. It is unlikely that an underbite will improve on its own at this point. However, there is a chance that your dog’s underbite can worsen due to poor oral hygiene and neglecting the condition.
Most dogs that show underbite symptoms as a young puppy will likely have a dog underbite for the rest of their lives. This misalignment can sometimes self-correct as your dog develops, but if your dog is genetically predisposed, it is highly unlikely for this to happen. Dog underbite can be corrected through surgery and braces in some cases.
Genetics, accidents, dental or skeletal problems can lead to underbites in dogs. In some breeds, underbites are the result of intentional breeding practices. Breeders breed underbite dogs specifically to engineer the type of jaw structure of a bulldog or a boxer.
An underbite malocclusion can be considered normal and healthy as long as the dog can chew and eat solid food comfortably and their bite is functional. Some breeds of dogs, usually flat-faced or brachycephalic, are naturally born with underbites. These breeds have been genetically bred to have a lower jaw that is slightly longer than the upper.
Bulldogs have brachycephalic skulls, which means their faces are pushed inward. As a result, the upper jaw is usually shorter than the lower — underbite. In some bulldogs, the underbite is minor, while in others, it is extreme that they find eating difficult.
As a responsible underbite dog parent, you need to be proactive in checking your dog regularly for any developments that could cause substantive health and dental issues so they can live a long and healthy life by your side.

Undershot is a class III malocclusion that is also referred to as mandibular prognathism, maxillary brachygnathism, mandibular mesioclusion, or an underbite. This malocclusion is characterized by a shorter upper jaw and a longer lower jaw, resulting in lower teeth that are in front of the upper teeth. While this condition is normal for some breeds, such as Bulldogs, in many breeds it is unusual. An undershot jaw occurs when the lower jaw grows faster than normal and becomes longer than the upper jaw, and is usually evident around 8 weeks of age in puppies. This misalignment can cause soft tissue trauma, such as to the lips. When the incisors meet instead of fitting next to each other, it is called a level bite. When the malocclusion causes the lower incisors to be placed in front of the upper incisors, it is called a reverse scissors bite.
The cause of overshot and undershot jaws in dogs relate to the increased or decreased rate of growth of the upper and lower jaws in relation to one another. This can occur due to a: Genetic disorder Trauma; Systemic infection ;Nutritional disorder; Endocrine disorder; Abnormal setting of puppy teeth; Early or late loss of puppy teeth.
After a quick physical exam, your vet may have to sedate your dog in order to perform a thorough oral exam. This will assess your dog’s skull type and teeth location in relation to the teeth on the opposite jaw. Often, the placement of the upper and lower incisors in relation to one another can determine what type of malocclusion your dog has. Your vet will note any areas of trauma due to teeth striking those areas, and any cysts, tumors, abscesses, or remaining puppy teeth that may be present. A dental X-ray can also help to assess the health of the jaws and teeth. These diagnostic methods will lead to a diagnosis of an overshot or undershot jaw in your dog.
Treatment of a jaw misalignment will depend on the severity of the condition. If your dog has a misalignment, but can still bite and chew food without problems, no treatment may be needed. If the misalignment is caught early in a puppy’s life, it may only be temporary and may correct itself over time. However, there are times when intervention may be needed. If your puppy’s teeth are stopping the normal growth of his jaws, then surgery to remove those puppy teeth may be performed. This may allow the jaws to continue to grow, but will not make them grow. For older dogs who are experiencing pain and trauma due to misaligned jaws and teeth, oral surgery is generally performed to extract teeth that are causing trauma, to move teeth so that they fit, or to create space for a misaligned tooth to occupy. Other therapies include crown reductions or braces.
If your dog is genetically programmed to have an overshot or undershot jaw, intervention can help, but will not slow or stop the abnormal growth of either jaw. Prevent jaw misalignments in puppies by not breeding dogs who have overshot or undershot jaws.

You can download this article on puppy teeth problems as an ebook free of charge (and no email required) through the link below. This comprehensive article covers such topics as malocclusions, overbites, underbites and base narrow canines in dogs. Special emphasis is placed on early intervention – a simple procedure such as removing retained puppy teeth can save many problems later on.
One of the biggest misconceptions is that dental problems don’t need the same treatment in animals as they do in humans. Nothing could be further from the truth! Dogs’ teeth have the same type of nerve supply in their teeth as we do, so anything that hurts us will hurt them as well.
All dogs, whether they are performance dogs or pets, deserve to have a healthy, pain-free mouth. Oral and dental issues frequently go undiagnosed in dogs, partly because the disease is hidden deep inside the mouth, and partly because dogs are so adept at hiding any signs of pain. As a pack animal, they don’t want to let the rest of the pack (including us!) know they have a problem, as anything that limits their usefulness to the pack may be grounds for exclusion. This is a survival instinct. Dogs will suffer in silence for as long as they can, and they only stop eating when they cannot bear the pain any longer.
This article has been written to help you understand how oral and dental problems develop in puppies, what the implications of these issues are, and what options are available to you and your pup to achieve the best outcomes in terms of overall health, comfort and performance. You don’t need to read it from top to bottom, as your dog would need to be pretty unlucky to need all the advice included here!
However, I do recommend that you look through the information on what a ‘normal’ mouth is, as this will help you to understand how each problem can arise.
baby) teeth which erupt between 3-8 weeks of age. These are replaced by the adult (permanent) teeth between 4-7 months of age. Adult dogs should have a total of 42 teeth. The difference in the number of deciduous and adult teeth arises because some adult teeth (the molars and first premolars) don’t have a deciduous version.
The ‘carnassial’ teeth are the large specialised pair of teeth towards the back of the mouth on each side, which work together like the blades of a pair of scissors. The upper carnassial is the fourth premolar, while the lower one is the first molar The upper jaw is the maxilla, and the lower jaw is the mandible.
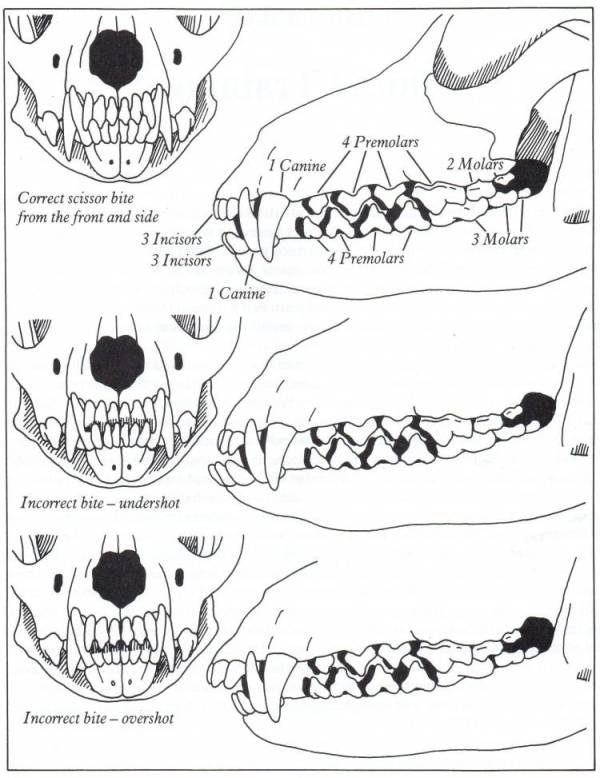
The way the teeth align with each other is referred to as the ‘occlusion’. Normally the upper incisors sit just in front of the lower incisors, this is called a ‘scissor bite’. The lower canines sit in the gap between the upper canines and corner (third) incisors, without rubbing against either of these teeth.
Although a scissor bite is standard for most breeds, in some breeds with a short, wide muzzle (brachycephalic skull type), a reverse scissor bite is accepted as the breed standard, where the upper incisors are behind the lower ones, and the lower canines are shifted forward. A level bite (where the upper and lower incisors are in line with each other) is also acceptable in some breeds.
The points of the smaller lower premolars should point to the spaces between the upper premolars, with the lower first premolar being the first from the front. The upper carnassial tooth should sit outside the lower carnassial tooth.
The bulk of the tooth is made up of dentine (or dentin), a hard bony-like material with tiny dentinal tubules (pores) running from the inside to the outside. In puppies, the dentine is relatively thin, making the tooth more fragile than in an older dog. The dentine thickens as the tooth matures throughout life.
The crown is covered in enamel, which is the hardest material in the body (even harder than bone!). This is only made prior to eruption, and cannot be regenerated if damaged.
Inside the tooth is the pulp, which is living tissue containing blood vessels, nerves and immune cells. The nerves have processes which extend through the dentinal tubules, and if these are exposed or stimulated they can cause sensitivity or intense pain.
Malocclusion is the termed used for an abnormal bite. This can arise when there are abnormalities in tooth position, jaw length, or both. The simplest form of malocclusion is when there are rotated or crowded teeth. These are most frequently seen in breeds with shortened muzzles, where 42 teeth need to be squeezed into their relatively smaller jaws. Affected teeth are prone to periodontal disease (inflammation of the tissues supporting the teeth, including the gums and jawbone), and early tooth loss.
Crowded upper incisor teeth in an English Bulldog, with trapping of food and debris. There is an extra incisor present which is exacerbating the problem.
Anterior (rostral) crossbite occurs when one or more upper incisors are positioned behind their lower counterparts. Constant striking of the lower incisors and oral tissues by the upper teeth may result in periodontal disease, pulpitis (inflammation of there sensitive living pulp tissue inside the teeth) and early tooth loss
‘Base narrow’ canines (Linguoverted or ‘inverted’ canines) are a relatively common and painful problem in Australian dogs. The lower canines erupt more vertically or ‘straight’ than normal (instead of being tilted outwards), and strike the roof of the mouth. This causes pain whenever the dog chews or closes its mouth, and can result in deep punctures through the palatal tissues (sometimes the teeth even penetrate into the nasal cavity!). In our practice in Sydney, we see this most commonly in Staffordshire Bull Terriers and Labrador Retrievers.
Lance’ canines (Mesioverted, hard or ‘spear’ canines) occur when an upper canine erupts so it is pointing forward, like a tusk. This is seen most commonly in Shetland Sheepdogs, and can lead to lip trauma and displacement of the lower canine tooth (which cannot erupt to sit in its normal position in front of the upper canine).
Class II malocclusions (‘overshot’) arise when the lower jaw is relatively short compared with the upper jaw. This type of occlusion is NEVER considered normal and can result in significant and painful trauma to the upper gums, hard palate and teeth from the lower canines and incisors.
Class III malocclusions (‘undershot’, ‘prognathism’) occur when the lower jaw is relatively long compared with the upper jaw. The upper incisors may either meet the lower ones (level bite) or sit behind them (reverse scissor bite). While this is very common, and considered normal for some breeds, it can cause problems if the upper incisors are hitting the floor of the mouth or the lower teeth (similar problems to rostral crossbite). If the lower canines are striking the upper incisors, the accelerated dental wear often results in dead or broken teeth.
Class IV malocclusions (‘wry bite’) occur when there is a deviation of one or both jaws in any direction (up and down, side to side or front to back). These may be associated with mild to severe problems with chewing, damage to teeth and oral tissues, and chronic pain.
Normal development of the teeth and jaws is largely under genetic control, however environmental forces such as nutrition, trauma, dental interlock and other mechanical forces can also affect the final outcome.
As the interaction between these factors can be quite complex, it is recommended that you have your pup individually assessed – feel welcome to call me for advice.
Most malocclusions involving jaw length (skeletal) abnormalities are genetic in origin. We need to recognise this as it has enormous implications if you are planning to breed, as once a malocclusion is established in a line, it can be heartbreaking work to try and breed it back out.
The exact genes involved in jaw development are not yet well understood. We do know that the upper and lower jaws grow at different rates, at different times, and are under separate genetic control. In fact, the growth of one only affects the growth of the other if there is physical contact between them via the teeth. This contact is called ‘dental interlock’.
When the upper and lower teeth are locked against each other, the independent growth of either jaw is severely limited. This can occasionally work in the dog’s favour, for example if the lower jaw is slightly long compared with the upper jaw, the corner incisors may lock the lower canines in position behind them, limiting any further growth spurts of the lower jaw.
However, in many cases, dental interlock interferes with jaw development in a negative way. A classic example we see regularly in our practice is when a young puppy has a class II malocclusion (relatively short lower jaw) and the lower deciduous canines are locked behind the upper deciduous canines, or trapped in the tissues of the hard palate. In these cases, even if the lower jaw was genetically programmed to catch up to the upper jaw, it cannot physically do so.
Early removal of the lower canines (and often the lower incisors as well) to relieve this problem is strongly recommended. This procedure is called ‘interceptive orthodontics’ as we are ‘intercepting’ the developing problem before growth is completed and it is too late.
Extraction of these teeth will not stimulate jaw growth, but will allow it to occur if nature (ie genetic potential) permits. It also relieves the painful trauma caused by the teeth to the hard palate whenever the pup closes its mouth (and we all know how sharp those baby teeth are!!). More information on interceptive orthodontics can be found later in this book.
In some breeds, a genetic tendency for retained deciduous teeth can also contribute to the development of problems, such as anterior crossbite seen in several of the toy breeds.
It is crucial to remember that genetic malocclusions are not usually seen in all puppies in an affected litter as they are not dominant traits. Puppies can carry the genes contributing to genetic faults without showing any physical signs at all. If an affected puppy is noted, extreme caution should be exerted when planning future breeding from the parents and siblings, and neutering of the affected puppy is strongly recommended.
Although diet often gets the blame for development of malocclusions, the role of nutrition is actually much less significant than is often believed. Obviously gross dietary deficiencies will affect bone and tooth development, for example severe calcium deficiency can lead to ‘rubber jaw’. However, the vast majority of puppies are on balanced, complete diets and have adequate nutrient intake for normal bone and tooth development.
One myth I have heard repeated by several owners is that strict limitation of a puppy’s dietary intake can be used to correct an undershot jaw. This is simply NOT true. Limiting calories will NOT slow the growth of the lower jaw relative to the upper jaw (both jaws receive the same nutrient supply). Such a practice is not only ineffective, it can be detrimental for the puppy’s overall growth and development.
Trauma, infection and other mechanical forces may affect growth and development of the jaws and teeth. Developing tooth buds are highly sensitive to inflammation and infection, and malformed teeth may erupt into abnormal positions (or not erupt at all!). Damage to developing teeth can also occur if the jaw is fractured.
Retained or persistent deciduous (puppy) teeth can also cause malocclusions by forcing the erupting adult teeth into an abnormal position. As previously mentioned, this may be a genetic trait, but can also occur sporadically in any breed of dog.
A full bite assessment can help differentiate between malocclusions which are due to shifting of teeth alone, and those which have an underlying genetic basis. Contact me if you would like to arrange a bite assessment for your puppy
The basic rule is that every dog deserves a pain-free, functional mouth. If there is damage occurring to teeth, or oral tissues, we need to alleviate this, to allow the dog to live happily and healthily. If there is no functional problem and no trauma occurring, then treatment is simply not required.
Sometimes the hardest part is determining whether the problem is in fact causing pain. As we know, dogs are very adept at masking signs of oral pain, and will and will continue to eat despite real pain. Puppies, in particular, don’t know any better if they have had pain since their teeth first erupted very early in life.
Early assessment to determine whether intervention is required is critical in puppies with any signs of occlusal problems. Not only does this allow us to relieve their pain promptly, it can allow for easier correction of problems than if we wait until the permanent teeth have fully erupted and settled into place.
The overriding aim is always to give the dog a healthy, pain-free and functional mouth. Sometimes this will result in a ‘normal’ mouth, whereas in other cases, this might not be realistically achievable.
While some basic advantages and disadvantages of the different treatment options are outlined here, it is very important to seek specific advice for your individual dog, as no two mouths are exactly the same, and an individual bite assessment will help us determine the best course of action together. You can contact us anytime.
Malpositioned teeth may be moved into a more appropriate position using orthodontic appliances such as braces (yes, braces), wires, elastic (masel) chains or plates (similar to those used in humans!). In some cases, this may be a multi-step procedure which means repeated general anaesthetics.
Extraction of lower canine teeth – the roots of these teeth make up about 70% of the front of the jaw, and so there is a potential risk of jaw fracture associated with their removal. Some dogs also use these teeth to keep the tongue in position, so the tongue may hang out after extraction.
Extraction of teeth may severely limit an animal’s success in the show ring, especially in breeds where the correct number of teeth is emphasised in the breed standard.
Orthodontic movement of teeth is a complicated science, and, while some procedures appear quite straightforward, permanent damage to teeth and the surrounding structures can result from inappropriate procedures, poorly fitted appliances, or excessive pressures.
The outdated practice of using rubber bands to move the teeth is not recommended, as they slip down between the tooth and the gum, causing damage to the sensitive tissue here. The forces applied are also difficult to regulate, which can cause damage to the ligaments around the teeth, as well as the tooth roots. Much safer and more effective methods are now available.
Procedures to alter the shape of the teeth and make them fit better in the mouth can also be performed. This may vary from removal of small amounts of enamel (odontoplasty) to create space between teeth, right through to shortening the crown of a tooth to prevent it from causing trauma (crown reduction).
Crown reduction is commonly performed to treat base narrow canines, or class II malocclusions, where the lower canines are puncturing the hard palate. Part of the tooth is surgically amputated, a dressing inside the tooth to promote healing and the tooth is sealed with a white filling (just like the ones human dentists use). This procedure MUST be performed under controlled conditions as it exposes the highly sensitive pulp tissue. If performed incorrectly, the pulp will become infected and extremely painful for the rest of the dog’s life.
This pup has trauma in the roof of her mouth due to her left lower canine. A crown reduction procedure relieves the trauma while maintaining some functionality and avoiding extraction.
Even the less invasive odontoplasty (enamel shaping) can result in exposure of the sensitive dentine or pulp tissue if taken too far, and must be performed with extreme care to avoid permanent problems. Xrays are recommended prior to surgery so we can measure how far we can go before we get into the ‘danger zone’.
Although sometimes practised, clipping the tips of the teeth of puppies is NOT a humane procedure, and not only causes intense pain (imagine how it would feel if your own tooth was cut in half), but the resulting pulp infection can cause irreversible damage to the adult tooth buds which are developing underneath.
Extraction of teeth is sometimes performed, alone or in combination with other orthodontic treatments. This may be the preferred treatment in cases where:
While the dog may lose some function, this is far preferable to doing nothing (this condemns the dog to a life of pain). Indeed, unless released into the wild, dogs do well even if we need to extract major teeth (canines and carnassials), as they have the humans in their pack to do all the hunting and protecting for them.
This is the term we use when we remove deciduous teeth to alter the development of a malocclusion. The most common form of this is when we relieve dental interlock that is restricting normal jaw development. Such intervention does not make the jaw grow faster, but will allow it to develop to its genetic potential by removing the mechanical obstruction.
Extraction of deciduous lower canines and incisors in a puppy with an overbite releases the dental interlock and gives the lower jaw the time to ‘catch up’ (if genetically possible).
As jaw growth is rapid in the first few months of life, it is critical to have any issues assessed and addressed as soon as they are noticed, to give the most time for any potential corrective growth to occur before the adult teeth erupt and dental interlock potentially redevelops. Ideally treatment is performed from eight weeks of age.
Extraction of deciduous teeth is not necessarily as easy as many people imagine. These teeth are very thin-walled and fragile, with long narrow roots extending deep into the jaw. The developing adult tooth bud is sitting right near the root, and can be easily damaged. High detail intraoral (dental) xrays can help us locate these tooth buds, so we can reduce the risk of permanent trauma to them. Under no circumstances should these teeth be snapped or clipped off as this is not only inhumane, but likely to cause serious infection and ongoing problems below the surface.
Permanent enamel damage on adult teeth following extraction od deciduous teeth. The risk of this can be minimised by use of dental x-rays and extremely good surgical technique.
The aim of any veterinary procedure should always be to improve the welfare of the patient, so the invasiveness of any treatment needs to be weighed up against the likely benefits to the dog. Every animal deserves a functional, comfortable bite, but not necessarily a perfect one. Indeed, some malocclusions (particularly those involving skeletal abnormalities) can be difficult to correct entirely.
In addition to the welfare of the individual dog, both veterinarians and breeders need to consider the overall genetic health of the breed. Both the Australian National Kennel Club and (in New South Wales where our practice is situated) the Veterinary Practitioners’ Board stress that alteration of animals to conceal genetic defects for the purpose of improving their value for showing (and breeding) is not ethical.
For animals with malocclusions, very strong consideration needs to be paid to whether or not breeding from the affected animal is in the interests of improving the breed. If there is a genetic component, then neutering or selective breeding is recommended. As the vast majority of orthodontic abnormalities are not dominant in their inheritance (not all pups carrying the ‘bad’ genes will have visible problems), a ‘small’ issue seen sporadically can easily become widespread within a line.
This not only means many pups will have physical problems requiring correction for their own individual welfare, but breeding the problem out again can be extremely difficult.
The bottom line is that, while all dogs will have multiple treatment options available, and in some cases the occlusion can be corrected to the point of being ‘good for show’, advice should definitely be sought about the likelihood of a genetic component prior to embarking upon this, as the consequences for the breed can be devastating if such animals (or their close relatives) become popular sires or dams.
Sometimes a puppy may be missing one or more teeth. In the absence of trauma (which is usually apparent for other reasons!), there are a couple of things that may be going on.
Sometimes a tooth is congenitally missing, that is it has never developed. While dogs can physically cope well with missing teeth, in some breeds this is considered a serious fault, and will severely affect the chances of the dog being successful in the show ring.
Alternatively, a ‘missing’ tooth may be unerupted below the gumline. This can only be diagnosed using xrays. In some cases, the tooth may be trapped under a thickened layer of gum tissue, and surgery to relieve the obstruction (an operculectomy) may allow the tooth to erupt smoothly into the correct position if performed early enough.
Impacted lower canines trapped under thick gum tissue. They are also in a base narrow position. These teeth were able to erupt when tissue was surgically released (operculectomy).
Sometimes, the tooth will be in a favourable position but caught behind a small rim of jawbone – again early surgical intervention may be successful in relieving this obstruction. If the tooth is in an abnormal position or deformed, it may be unable to erupt even with timely surgery.
Impacted or embedded teeth should be removed if they are unable to erupt with assistance. If left in the jaw, a dentigerous cyst may form around the tooth. These can be very destructive as they expand and destroy the jawbone and surrounding teeth. Occasionally these cysts may also undergo malignant transformation (ie develop into cancer).
Firstly, if there are two teeth in one socket (deciduous and adult), the surrounding gum cannot form a proper seal between these teeth, leaving a leaky pathway for oral bacteria to spread straight down the roots of the teeth into the jawbone. Trapping of plaque, food and debris between the teeth also promotes accelerated periodontal disease. This not only causes discomfort and puts the adult tooth at risk of early loss, but allows infection to enter the bloodstream and affect the rest of the body.
If the deciduous tooth is still firmly in position as the adult tooth is erupting, it forces the adult tooth into an abnormal position which can cause a significant malocclusion. For example, the lower adult canines normally erupt on the inside of the deciduous teeth, so if they are forced to erupt alongside them, a painful base narrow malocclusion can result.
The upper adult canines normally erupt in front of the deciduous ones, so forcing them further forward can result in ‘lance’ canines. Finally, the upper adult incisors usually erupt behind their deciduous versions, so if these are retained a rostral crossbite may develop.
Retained upper baby canines force the adult canines to erupt in a more forward position. This can close the gap where the lower canine usually sits, forcing it into a traumatic position.
Puppies play rough, chew whatever they can get hold of, and have tiny teeth with very thin walls. Therefore fractures will sometimes occur. A common misconception is that broken deciduous teeth can be left until they fall out. Unfortunately this is NOT true. From the puppy’s point of view, broken teeth HURT, just as they do in children. Anyone who has had a bad toothache would agree that even a few weeks is a long time to wait for relief!
Broken teeth also become infected, with bacteria from the mouth gaining free passage through the exposed pulp chamber inside the tooth, deep into the underlying jawbone. This is not only painful, but can lead to irreversible damage to the developing adult tooth bud, which may range from defects in the enamel (discoloured patches on the tooth) through to arrested development and inability to erupt. The infection can also spread through the bloodstream to the rest of the body. Waiting for the teeth to fall out is NOT a good option!
We cannot rely on dogs to tell us when they have oral pain. It is up to us to be vigilant and watch for signs of developing problems. Train your pup to allow handling and examination of the mouth from an early age. We will be posting some videos of oral examination tips shortly, watch out in your email inbox for this. Things can change quickly – check their teeth and bite formation frequently as they grow.
Seek veterinary care as soon as a potential problem is noticed – you can call me on 1300 838 336 or email me anytime on support@sydneypetdentistry.com.au for advice or assistance.
Remember, early recognition and treatment is crucial if we want to keep your dog happy and healthy in and out of the show ring. The sooner we treat dental problems, the higher the chance of getting the best possible results with the least invasive treatment.
Granted, a perfectly aligned set of pearl whites is sought-after for a million-dollar smile in the human world. However, in the doggy world, having a canine malocclusion or underbite (misaligned teeth) is the least of their worries.
Depending on a pooch’s breed, an underbite is particularly regarded as the standard or could be a hereditary abnormality, which may usher in difficulties in eating, among other problems.
Nonetheless, knowledge is power! In this guide, we’ll explore the ins and outs of a dog underbite, including the causes, cost, and treatment. Knowing this can aid in the minimization of problems and curb the reoccurrence of irregular bites in bloodlines.
It describes a skeletal or dental condition characterized by the lower teeth protruding farther than the upper front teeth. A dog underbite is also known as a Class-3 malocclusion. In addition to creating an appearance in the face and mouth that closely resembles a bulldog, malocclusion triggers abnormal teeth alignment, which causes an irregular bite.
A pooch with a protruding lower jaw and bottom teeth sticking out when at rest is referred to as an underbite dog. Before we delve into whether or not underbite on pooches can be rectified, it’s essential to understand what causes it and its variations.
It’s probably the top cause of malocclusion in pooches. Dental underbite occurs when one or a few teeth are irregularly positioned within a regular facial skeletal structure. As puppies grow, they begin losing their milk teeth that are gradually substituted by the permanent ones.
However, in some instances, a puppy’s baby teeth don’t fall. Consequentially, they interfere with the permanent teeth that end up growing crookedly due to the lack of ample space. In relatively undershot bites, the incisors are the only teeth that contribute to the misalignment.
Nonetheless, the dental cause of a dog underbite is the easiest to rectify, provided that interceptive orthodontics (the extraction of primary teeth) is performed as soon as possible.
In some dog breeds, an underbite is a cherished quality that is part of the norm. For instance, pugs, boxers, Pekingese, and bulldogs are renowned for their brachycephalic features. In this scenario, an abnormal mouth bone structure may result in the maxillary incisors or teeth making irregular contact with the gums. Consequentially, this leads to adverse distress and damage to your canine’s gums and teeth.
With the irresistible shorter jaws and pushed-in faces that a multitude of people find adorable, the gap into which the teeth erupt is restricted, ushering in a malocclusion. Given that skeletal underbite in pooches is significantly more problematic than dental causes, this leads to the rapid development of periodontal disease.
In this case, malocclusion in pooches is hereditary, meaning the condition will likely be transmitted from one generation to another. Moreover, it’s acquired when something goes wrong during the growth and development or gestation stage, for instance, trauma or infection, among other events that stunt maxillofacial growth.
Typically, a dog’s lower and upper teeth intersect in a ‘scissor bite’ when the jaw is closed. However, some scenarios arise whereby the lower teeth stick out in front of the upper ones causing a reverse scissor bite. Genetic causes of a dog underbite are seen in long and medium-muzzled pooches.
In some scenarios, a puppy’s lower jaw grows more rapidly, becoming visibly longer than the upper jaw. Occurring in puppies as young as eight weeks, some upper jaw teeth get restricted behind those of the lower jaw. Consequentially, the upper jaw doesn’t grow at the normal rate.
At times, the case of a dog underbite is acquired from the inappropriate tugging and chewing during the delicate stage of teething. Puppies then develop bite issues whereby their growing teeth shift from their initial position.
To avoid this predicament, refrain from playing tug-of-war and other aggressive games with your dog. Using ropes or towels to delight in these games can result in your pet’s teeth shifting into an unusual position, which results in their misalignment.
Dogs with adverse undershot bites may experience challenges in chewing. Furthermore, their soft tissues get damaged. At times, the undershot bite is adverse enough to require tooth extraction or orthodontic treatment.
Inform your vet immediately you spot the development of an underbite in your puppy. Early intervention can make all the difference in curbing more adverse issues.
However, it’s more prevalent in certain breeds than others. Although small dog breeds with underbite are the most common, boxers and other larger breeds are also susceptible. Here are a few examples:
If your dog has an underbite and you’re scratching your head wondering whether it can be rectified, fret not, as the answer is yes! The good news is most dog types of underbite don’t call for any treatment if it’s not interfering with the chewing and swallowing process.
It’s typically used for altering and shortening crowns to curb the tooth from triggering trauma. Crown modification shifts the teeth into their appropriate positions.
It’s a procedure that encompasses the extraction, shifting, and shortening of teeth to ensure they perfectly fit like a puzzle and no longer hurt a dog.
Untreated underbite causes more than off-kilter smiles. As you may have guessed, dogs with malocclusion are susceptible to a wealth of health risks, as outlined below. It ushers in a life of discomfort for your beloved canine companion.
Granted, pooches with an underbite smile are as adorable as they come. However, this condition can trigger adverse oral problems, so it’s in the best interest of your pet to act as quickly as possible. If your pooch is exhibiting any of the symptoms mentioned above, we recommend visiting your local vet as soon as you can. They’ll then check for signs of infection and pain.
Upon examination, the vet will recommend treatment if need be. At times, an underbite doesn’t cause irritation, which should put you at ease. Nonetheless, ensure you request a type of X-ray known as a dental radiograph for your pet. It will easily pinpoint most oral ailments in dogs.
If you’re curious as to how much you’ll have to pay to correct your pup’s underbite, keep in mind that the orthodontic treatments vary based on various factors. They include the specific underbite condition, rounds of anesthesia, and the number of teeth involved. Typically, the price ranges from $1500 to $4000, after which your pet will need to visit the vet biweekly or weekly to monitor the progress.
Underbite in young dogs can be rectified using braces. Nonetheless, filling and extraction can also be applied. The treatment alternatives for a puppy with an underbite vary based on the type of malocclusion involved, their health status, and age.
As is the case with adult dogs, a puppy with an underbite is susceptible to health problems. If you notice an underbite, we recommend seeking medical attention to determine if it’s detrimental to their health. If you’re wondering whether your puppy will grow out of the underbite, the truth is, although it’s possible, the chances are slim to none if it’s genetic.
Symptomatic dog underbite can gain from early treatment and care to prevent eating challenges and pain, among other complications. With that being said, here’s a breakdown of a few ways to care for a pooch with an underbite.
We recommend switching from hard to soft food when residing with a pup with an underbite. After all, it’s a no-brainer that a dog underbite causes chewing problems.
Wet dog food is an excellent option as it puts minimal stress on your pooch’s teeth when eating. You can also consider soft, chewy, or baked dog treats.
Frequent cleaning is necessary to ensure a pup’s teeth remain in tip-top health. Therefore, brush your dog’s teeth with a vet-recommended toothpaste and toothbrush every two days.
A dog with an underbite typically develops excessive calculus and tartar. As such, targeting this build-up with dental formula water will keep your pooch’s gums and teeth in excellent condition.
While a dog underbite isn’t necessarily a problem, it’s undoubtedly a cause for concern. Turning a blind eye can usher in a boatload of health adversities for your pup, and that’s the last thing you need.
Therefore, as a responsible dog owner, you should be proactive in taking the steps we’ve discussed to pinpoint and treat an underbite for your pet to live a long, healthy, and happy life right by your side. Moreover, you need to exercise vigilance when it comes to planning regular checkups to monitor your pup’s health.
Lastly, without a shadow of a doubt, all pooches are worthy of equal care and love. However, we don’t recommend seeking out dog breeds that are susceptible to an underbite (regardless of how adorable they are) unless you can provide the much-needed care that includes hefty vet bills if complications crop up.

An overbite or class 2 malocclusion results in the lower canine teeth striking the roof of the mouth or palate. This is a painful condition. Dental therapy should be performed as soon as possible with the goal to provide a “comfortable and functional bite”.
Extraction therapy of puppy teeth is recommended as young as possible (6-9 weeks of age), to relieve the pain of tooth-to-palate contact as well as to allow the lower jaws to grow to their genetic potential. Unfortunately, most lower jaws will remain too short. Therefore, these pets must be re-evaluated at 5.5 months of age to select the best therapy: orthodontic therapy, extraction of the lower canine teeth or crown reduction (shortening the teeth) and pulp capping.

This condition is most often spotted at either the first or second puppy checks or between 6 and 8 months of age as the permanent (adult) teeth erupt. Either the deciduous or permanent lower canines occlude into the soft tissues of the roof or the mouth causing severe discomfort and, possibly, oral nasal fistulae.
The fact sheet answers many questions you may have about the cause of this problem and the various treatments available. It is important not to delay treatment of deciduous lower canines as the window of opportunity is only a matter of a few weeks until the permanent canines erupt at 22 to 26 weeks of age. A new problem can then present with bigger teeth causing more damage.
We advise you email us images of the teeth (mouth closed, lips up and side on for both left and right) just a few days before you travel. Things change quickly in growing dogs and it might save you a wasted journey.
This is an inherited condition - an autosomal recessive mutation. Both parents may look normal but carry recessive genes for the condition. When this genetic information is passed onto the litter, approximately one pup in four will be affected, appear abnormal and can pass the genetic information on if bred from. In addtion, two pups in four will carry an abnormal gene from one parent and a normal gene from the other. This pups will look normal but can pass the problem on if bred. Finally one pup in four will not be a carrier of abnormal genes, will be unaffected and cannot pass the trait on to future generations.
If this condition appears in the litter, the most responsible course of action is not to breed from the parents again - either as a pair or individually with others. As there is currently no test to identify this gene, selecting another mate may mean they too are recessive carriers. All the normal looking sibling pups are likely to also carry the recessive genes. It is wise that they too do not contribute to passing the problem back into the breed"s gene pool. In many affected breeds, the gene pool of breeding individuals to select from is very small. If recessive carriers are routinely mating then it is not long before increasing numbers of pups appear with this condition. Over four decades we have monitored the breeds treated here and it is disappointing to note that many previously unaffected breeds are now being seen on a regular basis.
When a pup is treated for this condition we routinely supply the Kennel Club with a Change of Conformation form so they can track the parental origin. We also ask for permssion to send a DNA swab to the Animal Health Trust. This is anonymously evaluated as part of a research programme to identify the exact genetic origin of the condition with the aim of a simple test becoming available to identify recessive carriers. In time this will allow owners of known recessive carriers to select a mate unaffected by the condition.
Owners with young puppies identified with this problem at first presentation are advised to have the deciduous lower canines removed as soon as possible. There are three reasons for this:
Firstly, and most importantly, these teeth are sharp and hitting the soft tissues of the palate. These pups cannot close their mouth without pain and often hold the mouth slightly open to avoid contact. This is not pleasant. See above for an example of the damage caused to the hard palate by this problem.
Secondly, the growth of the mandible is rostral from the junction of the vertical and horizontal ramus. If the lower canines are embedded in pits in the hard palate, the normal rostral growth of the mandible(s) cannot take place normally due to the dental interlock caused by the lower canines being embedded in hard palate pits. This can cause deviation of the skull laterally or ventral bowing of the mandibles (lower jaws).
Thirdly, the permanent lower canine is located lingual to the deciduous canine. This means that if the deciduous lower canines are in a poor position it is a certainty the permanent teeth will be worse. See the radiograph below. The deciduous canines are on the outside of the jaws and the developing permanent canines are seen in the jaw as small "hats". It is clear that the eruption path of the permanent canines will be directly dorsal and not buccally inclined as is normal.
For these three reasons it is advisable to surgically remove the lower canine teeth as soon as possible to allow maximum time between the surgery and the time the permanent teeth erupt at between 22 and 24 weeks of age. See our file for illustration of removal of deciduous canines.
The deciduous tooth root is three to four times longer than the visible crown and curved - often 2.5cm in length and curved. The root apex is often located below the third lower premolar. See middle and right images below with extracted deciduous tooth laid over extraction site.
The roots are very fragile and will break easily if unduly stressed during removal. A broken root needs to be identified and removed otherwise it continues to form a barrier to the eruption path of the permanent canine and can cause local infection.
The permanent successor tooth is located lingual to the deciduous tooth and wholly within the jaw at this stage. Any use of luxators or elevators on the lingual half of the deciduous tooth will cause permanent damage to the developing enamel of the permanent tooth. See the images below showing canines (and also the third incisor) with extensive damage to the enamel. The radiograph also shows how much damage can occur to the teeth - see the top canine and adjacent incisor. Some severely damaged teeth need to be extracted while other can be repaired with a bonded composite. This damage is avoidable with careful technique using an open surgical approach.
Surgery to remove the deciduous canines may not prevent to need for surgery on the permanent canines but, without it, few cases will resolve if left to nature. Many owners are reluctant to have young pups undergo surgery. Our view is that surgical removal of the lower deciduous canines will not guarantee the problem does not happen again when the permanent teeth erupt but without surgery the chances are very slim.
In a few selected cases - usually only very mild lingual displacement - we can consider placing crown extensions on the lower canines to help guide them into a more natural position. It carries some uncertainly and will not be suited or work in all cases. The images below show crown extensions on a young Springer Spaniel.
Please note that the use of a rubber ball to assist tipping of the deciduous lower canines buccally is not appropriate at this age and will not work - see below.
If the permanent teeth are lingually displaced the pup is usually older than 24 weeks. The trauma caused by the teeth on the soft tissues can be considerable with pain as a consequence.
Do not try ball therapy with deciduous (puppy) teeth. There are two main reasons for this. Puppy teeth are fragile and can easily break. More importantly, the adult canine tooth bud is developing in the jaw medial to the deciduous canine tooth (see radiograph above in the puppy section). If the deciduous crown tips outwards the root will tip inwards. This will push the permanent tooth bud further medial than it already is.
Ball therapy will only work with adult teeth and only in some cases where the lower canines have a clear path to be tipped sideways - laterally - through the space between the upper third incisor and canine. The window of opportunity can be quite short, around 6 weeks, and starts when the lower canine teeth are almost making contact with the hard palate.
If you are considering ball therapy ask your vet their opinion and get them to send us images of each side of the closed mouth from the side with mouth closed and lips up.
The size and type of the ball or Kong is critical. The ball diameter should be the distance between the tips of the two lower canine teeth plus 50%. Therefore if this distance is 30mm the ball diameter is 45mm. If the ball is too small it will sit between the lower canines and produce no tipping force when the pup bites down. Too large a ball can intrude the lower canines back into their sockets.
The owner needs to encourage play with the ball several times a day (6 - 8) or as often as they will tolerate with a short attention span. The ball should be only at the front of the mouth to go any good. If there are no positive results in six weeks a further veterinary evaluation is advised.
These permanent teeth can theoretically be treated by three options. Not all options are available to all cases. These options are described below and are either surgical removal of the lower canines teeth (and possibly incisors also), crown amputation and partial pulpectomy or orthodontics via an inclined bite plane bonded to the upper canines and incisors. The latter option may not be available to all dogs if the diastema (space) between the upper third incisor and canine is too small for the lower canines to move into or if the lower canines are located behind (palatal) to the upper canines.
This is a sterile procedure to reduce the height of the lower canine crown that exposes the pulp. It requires a removal of some pulp (partial coronal pulpectomy) and placement of a direct pulp capping.
This is a very delicate proce




 8613371530291
8613371530291