overshot teeth in stock

An overbite might not seem like a serious condition for your dog, but severely misaligned teeth can lead to difficulty eating, gum injuries and bruising, bad breath and different types of dental problems, including tooth decay and gingivitis. Fortunately, there are ways to help fix the problem before it becomes irreversible.
An overbite is a genetic, hereditary condition where a dog"s lower jaw is significantly shorter than its upper jaw. This can also be called an overshot jaw, overjet, parrot mouth, class 2 malocclusion or mandibular brachynathism, but the result is the same – the dog"s teeth aren"t aligning properly. In time, the teeth can become improperly locked together as the dog bites, creating even more severe crookedness as the jaw cannot grow appropriately.
Small overbites often correct themselves as the puppy matures, and brushing the dog"s teeth regularly to prevent buildup can help keep the overbite from becoming more severe. If the dog is showing signs of an overbite, it is best to avoid any tug-of-war games that can put additional strain and stress on the jaw and could exacerbate the deformation.
If an overbite is more severe, dental intervention may be necessary to correct the misalignment. While this is not necessary for cosmetic reasons – a small overbite may look unsightly, but does not affect the dog and invasive corrective procedures would be more stressful than beneficial – in severe cases, a veterinarian may recommend intervention. There are spacers, braces and other orthodontic accessories that can be applied to a dog"s teeth to help correct an overbite. Because dogs" mouths grow more quickly than humans, these accessories may only be needed for a few weeks or months, though in extreme cases they may be necessary for up to two years.
If the dog is young enough, however, tooth extraction is generally preferred to correct an overbite. Puppies have baby teeth, and if those teeth are misaligned, removing them can loosen the jaw and provide space for it to grow properly and realign itself before the adult teeth come in. Proper extraction will not harm those adult teeth, but the puppy"s mouth will be tender after the procedure and because they will have fewer teeth for several weeks or months until their adult teeth have emerged, some dietary changes and softer foods may be necessary.

Enzo is a short-haired Havanese and he was born with his lower jaw shorter than the upper jaw. This is called an Overbite, also referred to as an Overshot Jaw, a Parrot Mouth or Mandibular Brachygnathism. This malocclusion is a genetic change and can be seen in a number of breeds, oftentimes collie related breeds and dachshunds. Occasionally this change happens because of differences in the growth of the upper and lower jaws, and in many cases it doesn’t cause any significant problems other than cosmetically.
Dr. Robin Riedinger evaluated Enzo at his first visit when he was just 11 weeks of age and while the lower jaw was too short, there was no evidence of damage and no indication that this was causing a problem for Enzo. When there is abnormal occlusion of the teeth, it is important to monitor closely for trouble caused by the teeth being aligned improperly. Malocclusions can lead to gum injuries, puncturing of the hard palate, abnormal positioning of adjacent teeth, abnormal wear and bruising of the teeth, permanent damage and subsequent death of one or more teeth, and in the long run, premature loss of teeth. Some malocclusions can be severe enough to interfere with normal eating and drinking.
Within three weeks, when Enzo was only 3.5 months old, it was clear that our doctors would need to intervene. The left and right sides of Enzo’s upper jaw (maxilla) were growing at different rates because the lower canine teeth were being trapped by the upper canine teeth. This is called Dental Interlock. Because the teeth are ‘locked’ in place, the lower jaw cannot grow symmetrically and this creates a number of other problems. Early intervention is critical.
The solution for Dental Interlock is to extract the teeth from the shorter jaw; in this case, the lower ‘baby’ canines and thereby allow the lower jaw (mandible) to grow in the best way possible. This procedure is most effective when the Dental Interlock is discovered early and the extractions are performed quickly. In some cases, this can be as early as ten weeks of age. Dr. Riedinger consulted with a local veterinary dental specialist to confirm the treatment plan and to get advice on extracting the deciduous teeth without damaging the developing adult canines. Dental radiographs are essential to proper extraction technique and also to ensure that there are no other abnormalities below the gumline.
You can see how long the roots of the deciduous ‘baby’ teeth are. During normal growth, the body will begin to resorb the roots, making them loose, and allow them to fall out as the adult tooth begins to emerge. When we need to remove the deciduous teeth before they are loose, it can be quite tricky to remove the tooth carefully without breaking it and without injuring the adjacent teeth.
Once extracted, each deciduous canine tooth was about 2 centimeters long; the roots were about 1.5 centimeters. Many people are surprised to learn that the root of a dog’s tooth is so large – 2/3 to 3/4 of the tooth is below the gumline. This is one reason why it is so important to use radiographs to evaluate teeth on a regular basis, not just in a growing puppy. Adult teeth can, and frequently do, have problems that are only visible with a radiograph.
Enzo came through his procedure extremely well. He was given pain medications for comfort and had to eat canned foods and avoid chewing on his toys for the next two weeks to ensure that the gum tissue healed properly. As he continues to grow we will be monitoring how his jaw develops and Dr. Riedinger will also be watching the alignment of his adult canine teeth when they start to emerge around six months of age. Hopefully this early intervention will minimize problems for Enzo in the future.

Malocclusion is when a child’s teeth become crooked or crowded. The child may also have a problem with his or her bite. That means the teeth of the upper jaw don’t meet normally with the teeth of the lower jaw when the jaw is closed.
Children who suck their thumbs or fingers after age 5 have a greater chance of developing malocclusion. Children with a very small space between their baby teeth are at risk too. They may have problems with malocclusion when their permanent teeth come in. This is because the permanent teeth are larger and need more space.
Your child’s healthcare provider can often diagnose malocclusion with a full health history and physical exam. He or she will likely refer your child to a dentist or an orthodontist for full evaluation and treatment. Orthodontists are specially trained dentists. They treat the irregularities of the teeth, bite, and jaws.
The goal of treatment is to straighten the teeth and improve the look of your child’s smile. Treatment is sometimes done in phases depending on the extent of the malocclusion. It may include:
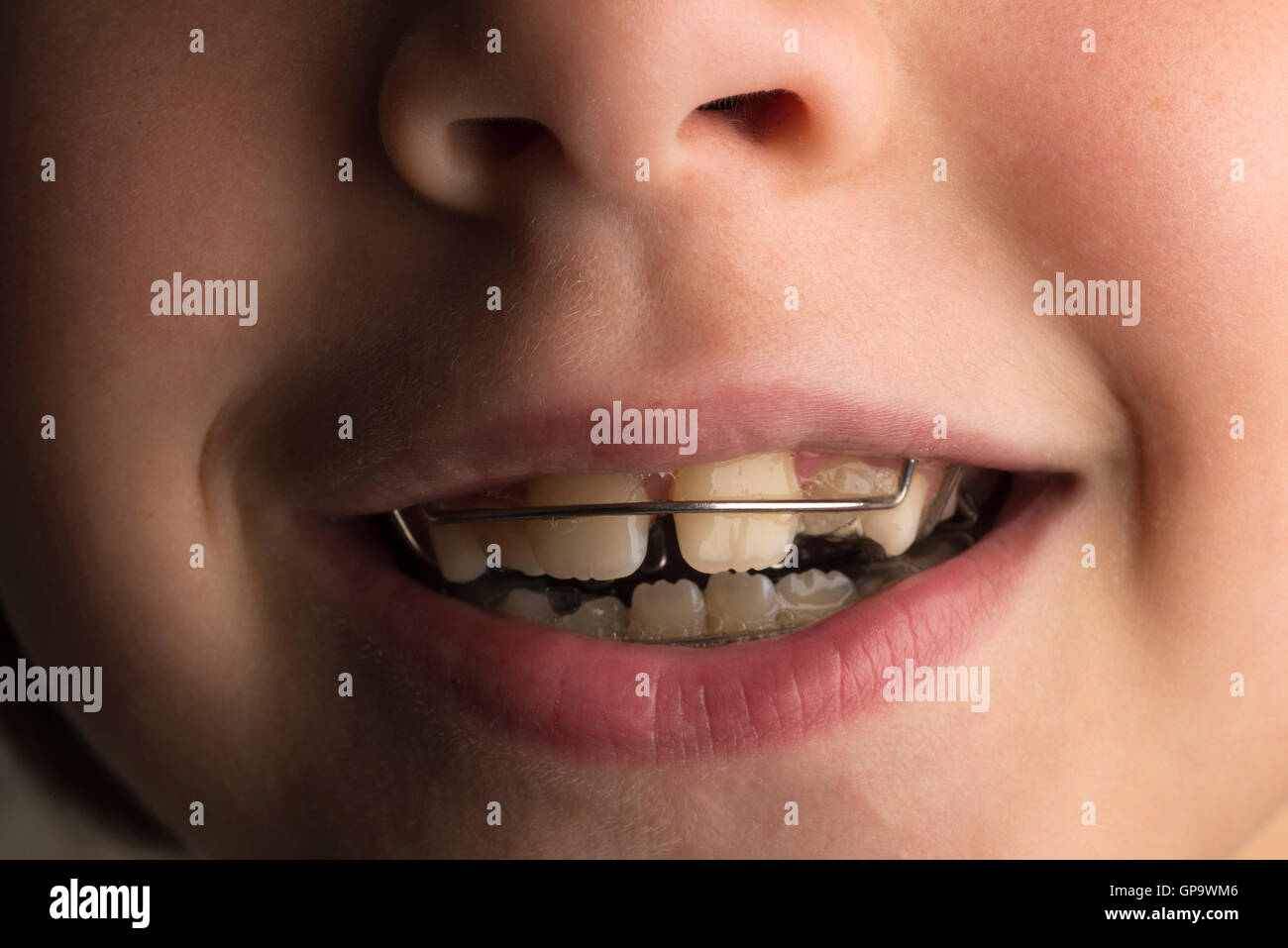
Mouth appliances.These may be removable (a retainer). Or they may be fixed (braces). A retainer is made of wires and plastic. It can be put in and taken out. It must be cleaned on a regular basis. Braces are small brackets attached to the teeth. They are connected with a wire. By tightening the wire from time to time, the orthodontist is able to slowly straighten the teeth over time.

Most people aren’t born with perfectly aligned teeth. Usually, slightly misaligned teeth don’t require any medical treatment. However, correcting an underbite, especially when it’s severe, can have big benefits.
Teeth will become easier to clean. Your risks for tooth decay and gum disease will decrease. You’ll also feel less strain on your teeth, jaws, and facial muscles.
Brushing and flossing your teeth regularly in addition to visiting a dentist for checkups and cleanings are important parts of treatment for healthy teeth. But those with an underbite or other dental issues must take special care of their teeth to prevent further damage and decay.
Brush your teeth at least twice a day for two minutes each time with toothpaste containing fluoride. Pay attention to brushing along your gumline and on the inside, outside, and the back of your mouth. Be sure you floss in addition to brushing. See your dentist at least twice a year for checkups and cleanings.
Medical treatment is the only way to truly correct an underbite and align teeth correctly. At the very least, medical treatment can improve the appearance of an underbite.
In less severe cases of underbite, a dentist may be able to use wire or plastic braces or other dental appliances to move the teeth into their correct place.
Removal of one or more teeth on the lower jaw may also help improve the appearance of an underbite if overcrowding of the teeth is contributing to the issue. A dentist may also use a grinding device to shave down or smooth teeth that are large or stick out.
The earlier an underbite is addressed, the better. If a child’s underbite is less severe, parents should wait until at least age 7 to seek corrective treatment such as braces. That’s when permanent teeth begin to erupt.

Normally, a kitten will have 26 baby teeth once it is six months old. By the time it reaches adulthood, an adult cat will have 30 teeth. Misalignment of a cat"s teeth, or malocclusion, occurs when the bite does not fit accordingly. That is, the top and bottom jaws do not fit together neatly. This may begin as the kitten"s baby teeth come in and usually worsens as their adult teeth follow.
The smaller front teeth between the canines on the upper and lower jaws are called incisors. These are used to grasp food and to keep the tongue inside the mouth. Canines (also known as cuspids or fangs) are found behind the front teeth, which are also used to grasp. Behind the canines are the premolars (or bicuspids) and their function is to shear or cut food. Molars are the last teeth and are found at the back of the mouth; they are used for chewing.
If problems with the palate persist, a fistula may result and become infected. In cases of misaligned teeth, the cat may have difficulty chewing, picking up food, and may be inclined to eat only larger pieces. They are also prone to tartar and plaque build-up.
With an overbite, the upper jaw is longer than the lower one. When the mouth is closed, a gap between the upper and lower incisors occurs. Kittens born with an overbite will sometimes have the problem correct itself if the gap is not too large. However, a cat"s bite will usually set at ten months old. At this time improvement will not happen on its own. Your pet"s overbite may worsen as the permanent teeth come in because they are larger and can damage the soft parts of the mouth. Teeth extractions are sometimes necessary.
Most bite malocclusions do not require treatment, but in some cases, extractions may be necessary. It’s a good idea to brush the teeth regularly to prevent abnormal build-up of tartar and plaque. Your veterinarian will recommend a dental specialist if you want to correct the teeth misalignment. In recent years, “braces” have been made for kittens to realign the teeth before they can become a health issue.

Although most young horses" mouths and teeth develop in a normal pattern, some horses are prone to an incorrect bite which occurs when the upper and lower incisors do not meet edge to edge as needed for effective chewing of hay and other feeds. This results in a malocclusion.
Both undershot jaw and overshot jaw are conditions of malocclusion. A malocclusion often results in poor digestion, and, in some cases, malnutrition because the horse has trouble eating or grazing and cannot chew feed well enough for good digestion.
Both undershot and overshot jaw are usually inherited. Many horses have slight malocclusions and the problem is serious only when the misalignment is so pronounced that the horse cannot graze and chew effectively, resulting in uneven wearing of the teeth and other dental problems.
Treatment of both undershot jaw and overshot jaw works best if detected by the time the horse is six months old. Wire tension bands from the upper incisors to the first maxillary cheek teeth to slow the growth of the upper jaw sometimes works well to correct overshot jaw.

Here, Paddy Dixon, MVB, PhD, MRCVS, professor of equine surgery in the University of Edinburgh’s Division of Veterinary Clinical Sciences, describes common problems horses encounter as their teeth develop, what problems these abnormalities cause, and treatment options.
“Many horses have some degree of overjet,” Dixon says. An overjet, also referred to as an overshot jaw, occurs when the chewing surfaces of the upper incisors (the front teeth) lie slightly in front of the chewing surfaces of the lower incisors. Most times, this slight misalignment does not cause ill effects to the horse.
“If very marked and left untreated in foals, cases of severe overjet may develop into overbite,” he cautions. This condition, commonly referred to as “parrot mouth,” occurs when all of the upper incisors lie in front of the lower incisors, resulting in excess tooth growth on the top row of teeth; this excess tooth growth can sometimes cause the horse to develop a smilelike appearance when the central upper incisors overgrow .
“Overjet and overbite are aesthetically undesirable but surprisingly, these problems rarely cause difficulty in prehension (grasping food),” Dixon notes. If the horse develops these smilelike incisors, veterinarian should evaluate and reduce the excess tooth gradually, ensuring that the underlying pulp is never exposed or overheated during the process. Most horses affected with overjet and overbite also have their top row of cheek teeth slightly in front of the lower cheek teeth, and thus, they develop overgrowths on the front of their first upper cheek tooth and the back of their last lower cheek tooth, as discussed below.
Dixon explained that with both underjet and overjet, the main clinical concern is a misalignment of the horse’s six cheek teeth (three molars and three premolars).
It’s a mouthful to say, and rostrally positioned (positioned closer to the nose) upper cheek teeth can cause a mouth full of problems for horses. Dixon explains that an imbalance in growth rates between maxillary (cheek bone) and mandibular (lower jaw) bone cause this disorder, which is “nearly always associated with incisor overjet or overbite.”
Several problems can arise from the upper cheek teeth being positioned further ahead than the lower ones. “Because the maxillary and mandibular cheek teeth rows are not in full occlusion (bite alignment), localized cheek teeth overgrowth–colloquially termed beaks, hooks, or ramps–develop on the front of the upper cheek teeth,” Dixon explains. “These overgrowths may be pushed against the lips and cheeks by the bit or noseband and so cause mucosal ulceration and bitting problems.”
Wry nose is a condition in which an affected foal’s upper jaw and nose are deviated, or turned to one side, Dixon explains. The teeth associated with this condition always have malocclusion (poor alignment), although most foals can still nurse and in most cases are bright and active.
This condition–in which one or more of an affected horse’s teeth do not develop–has the potential to affect both deciduous (baby) and permanent teeth, although “true” hypodontia most commonly affects permanent teeth, Dixon explains. And while a missing tooth might not seem like a major problem, Dixon explained that its absence can cause long-term damage to the horse’s mouth.
“Developmental hypodontia is relatively uncommon in horses, with the absence of equine teeth usually due to traumatic loss, disease, or age-related wear,” he explains. The main problem associated with missing teeth is overgrowth of the opposing tooth. In these cases overgrowth can be managed with semiannual dental care to prevent the overgrown teeth causing damage to surrounding structures
“The presence of supernumerary (additional) teeth is relatively uncommon in horses, usually developing in the permanent dentition,” says Dixon. He added that supernumerary teeth can be comprised of a single tooth or more than one tooth joined together.
“Equine supernumerary incisors may be more common–or possibly more readily identified–than supernumerary cheek teeth,” Dixon notes. Extra incisors often cause overcrowding and displacement of the normal teeth. In some cases he suggested it is possible to remove the additional teeth using sedation and nerve blocks. “If (the supplemental teeth are) interwoven amongst the other incisors, differentiation of supernumerary and normal teeth is difficult and safe extraction may be impossible,” he notes. In these cases regular veterinary dental care can help keep the horse’s mouth as healthy as possible.
Supernumerary cheek teeth are relatively uncommon in horses and can cause overcrowding and irregular spacing between teeth leading to periodontal disease. Treatment depends on the location of the supernumerary teeth and what problems they cause, he noted. Following careful clinical examination and radiography (X rays), common treatment options include extracting the additional tooth, widening or filling abnormal interdental spaces (that develop painful food packing), and reducing overgrowth.
“Dysplasia, or abnormal development of teeth, can involve the crown, roots, or all parts of the tooth,” Dixon says. “Dysplasias in the gross anatomy include dilacerations (abnormal bending of teeth), double teeth, abnormalities of size, and concrescence (roots of adjacent teeth joined by cementum) of teeth.”
Additionally, he notes that teeth can develop either too large (macrodontia) or too small (microdontia). Amelogenesis imperfecta (a tooth development disorder in which teeth are covered with thin, abnormally formed enamel) is another rare dental disorder in horses, Dixon added.
“Some cases of ‘stepmouth’ and ‘wave mouth’ are caused by mismatched eruption times of opposing permanent cheek teeth, allowing overgrowth of the teeth which erupt first,” Dixon explains.
Smaller and miniature breeds have this type of disorder more commonly than other breeds due to a likely mismatch between the size of their teeth and of the support bones (jaws), Dixon noted, and the steplike or wavelike overgrowths can remain–or even increase in size–throughout an affected horse’s lifetime.
Dixon notes that both deciduous incisors and cheek teeth can be retained past their normal time of shedding. In some cases, he noted, this will cause the permanent tooth to emerge into a displaced position adjacent to the retained deciduous tooth. The newly erupted tooth is often not fully aligned with its opposite tooth and so develops an overgrowth that can even cause chewing restrictions.
In most cases, Dixon says, these retained deciduous teeth can be readily identified and removed. However, it is sometimes advisable to have a veterinarian take a radiograph prior to extraction to ensure the additional tooth is not of the supernumerary variety.
Light breeds and miniature horses are also prone to developing cheek teeth vertical impactions (teeth that are too tightly squeezed by their neighbors and cannot freely erupt into the mouth) when permanent teeth are emerging. However, many larger breeds such as Thoroughbreds also develop this problem. They most commonly cause painless swelling on the bottom of the lower jaw (i.e., eruption cysts, or “3-year-old bumps” and “4-year-old bumps”) that usually disappear after a year or so, because “as the jaw bones lengthen, the impacted cheek teeth have room to erupt normally,” Dixon says.
If there is not enough room for the fourth cheek tooth to erupt normally at one year of age or for the fifth cheek tooth to erupt at two years of age, the (overcrowded) erupting tooth might be displaced and cause a potentially lifelong problem. The displaced tooth might then grow toward the cheeks or tongue, causing painful inflammation, but the most significant problem will be the presence of diastemata (space) between the normal teeth row and the displaced tooth. At these sites, food invariably becomes impacted and the horse can develop painful periodontal disease. If the displacement is very severe, a veterinarian might extract the displaced teeth–a procedure most readily performed in older horses, especially when deep periodontal disease is present.
This condition is most often spotted at either the first or second puppy checks or between 6 and 8 months of age as the permanent (adult) teeth erupt. Either the deciduous or permanent lower canines occlude into the soft tissues of the roof or the mouth causing severe discomfort and, possibly, oral nasal fistulae.
The fact sheet answers many questions you may have about the cause of this problem and the various treatments available. It is important not to delay treatment of deciduous lower canines as the window of opportunity is only a matter of a few weeks until the permanent canines erupt at 22 to 26 weeks of age. A new problem can then present with bigger teeth causing more damage.
We advise you email us images of the teeth (mouth closed, lips up and side on for both left and right) just a few days before you travel. Things change quickly in growing dogs and it might save you a wasted journey.
Firstly, and most importantly, these teeth are sharp and hitting the soft tissues of the palate. These pups cannot close their mouth without pain and often hold the mouth slightly open to avoid contact. This is not pleasant. See above for an example of the damage caused to the hard palate by this problem.
Thirdly, the permanent lower canine is located lingual to the deciduous canine. This means that if the deciduous lower canines are in a poor position it is a certainty the permanent teeth will be worse. See the radiograph below. The deciduous canines are on the outside of the jaws and the developing permanent canines are seen in the jaw as small "hats". It is clear that the eruption path of the permanent canines will be directly dorsal and not buccally inclined as is normal.
For these three reasons it is advisable to surgically remove the lower canine teeth as soon as possible to allow maximum time between the surgery and the time the permanent teeth erupt at between 22 and 24 weeks of age. See our file for illustration of removal of deciduous canines.
The permanent successor tooth is located lingual to the deciduous tooth and wholly within the jaw at this stage. Any use of luxators or elevators on the lingual half of the deciduous tooth will cause permanent damage to the developing enamel of the permanent tooth. See the images below showing canines (and also the third incisor) with extensive damage to the enamel. The radiograph also shows how much damage can occur to the teeth - see the top canine and adjacent incisor. Some severely damaged teeth need to be extracted while other can be repaired with a bonded composite. This damage is avoidable with careful technique using an open surgical approach.
Surgery to remove the deciduous canines may not prevent to need for surgery on the permanent canines but, without it, few cases will resolve if left to nature. Many owners are reluctant to have young pups undergo surgery. Our view is that surgical removal of the lower deciduous canines will not guarantee the problem does not happen again when the permanent teeth erupt but without surgery the chances are very slim.
If the permanent teeth are lingually displaced the pup is usually older than 24 weeks. The trauma caused by the teeth on the soft tissues can be considerable with pain as a consequence.
Do not try ball therapy with deciduous (puppy) teeth. There are two main reasons for this. Puppy teeth are fragile and can easily break. More importantly, the adult canine tooth bud is developing in the jaw medial to the deciduous canine tooth (see radiograph above in the puppy section). If the deciduous crown tips outwards the root will tip inwards. This will push the permanent tooth bud further medial than it already is.
Ball therapy will only work with adult teeth and only in some cases where the lower canines have a clear path to be tipped sideways - laterally - through the space between the upper third incisor and canine. The window of opportunity can be quite short, around 6 weeks, and starts when the lower canine teeth are almost making contact with the hard palate.
The size and type of the ball or Kong is critical. The ball diameter should be the distance between the tips of the two lower canine teeth plus 50%. Therefore if this distance is 30mm the ball diameter is 45mm. If the ball is too small it will sit between the lower canines and produce no tipping force when the pup bites down. Too large a ball can intrude the lower canines back into their sockets.
These permanent teeth can theoretically be treated by three options. Not all options are available to all cases. These options are described below and are either surgical removal of the lower canines teeth (and possibly incisors also), crown amputation and partial pulpectomy or orthodontics via an inclined bite plane bonded to the upper canines and incisors. The latter option may not be available to all dogs if the diastema (space) between the upper third incisor and canine is too small for the lower canines to move into or if the lower canines are located behind (palatal) to the upper canines.
Radiograph left lower canine before (left) and immediately after (right) surgery. Note the immature morphology of the canine teeth - thin walls and open root apices.
In order to monitor this process of maturation we need to radiograph these teeth twice at 4-6 months post-op and again at 12 -16 weeks post-op. This is a mandatory check. The quoted success reate of 92% implies 8% failure. Half of those to fail in the Luotonen study happened over a year post-op. To ensure any failure of maturity is identified we will not perform this surgery unless the owner agrees to this.
Normally a composite resin bite plane is bonded onto the upper teeth (see below) with an incline cut into the sides. The lower canine makes contact with the incline when the mouth closes and, over time, the force tips the tooth buccally. This takes around four to eight weeks. The lower canine will often migrate back into a lingually displaced position when the bite plane is removed. This can occur if the tooth height of the lower canine is too short (stunted). If the lower canine is not self-retained by the upper jaw when the mouth is shut further surgery may be required.

An overbite is when the top jaw and teeth overlap the lower jaw and teeth. Dentists and orthodontists refer to overbites as a type malocclusion. An overbite may be vertical or horizontal. A vertical overbite is where the top teeth overlap the bottom and a horizontal overbite has the top teeth protruding over the bottom teeth (more commonly known as overjet). Some patients can have signs of both.
An overbite can also be classified as being dental or skeletal. A dental overbite is when the teeth are in the wrong position and skeletal means the jaw causes the overbite. Overbites are the most common dental disorder in children.
It’s not clear why one person develops an overbite and another doesn’t. Some people are born with malformed jaws that develop unevenly. Others may be born with a jaw that is too big or too small for the teeth resulting in crowding or large spaces and an overbite. We know that genetics play a major part so if the parents needed orthodontic treatment for an overbite, it’s more likely their children will need treatment for similar problems.
Some of the deepest overbites are due to the environment rather than genetics. A child that consistently has a dummy or sucks their thumb or finger/s regularly past the age of five is at risk of pushing the bone and front teeth forward. The top teeth and jaw grow outwards to accommodate the forward tongue while the dummy or parts of the hand can push the bottom teeth and bone back. Encouraging a child to stop thumb sucking from five is important for allowing the jaw and teeth to develop as they should.
Even when a person passes childhood with no sign of an overbite, it could still develop as a teen or adult. Chewing fingernails, biting a pen consistently or losing teeth with no follow up treatment can cause an overbite later in life.
Braces are effective for treating most overbite problems. As part of the assessment stage, x-rays help determine the overbite type and the relationship between the teeth and jaw. Braces are then attached to the top and lower arches of the teeth.
The arch wire first straightens and aligns the teeth. During the second stage of braces, elastics (small rubber bands) may be used to slowly shift the jawline into the correct position. The bands are fitted on the brackets from top to bottom or front to back to help move the teeth and jaw. The bands are removed before eating, drinking and brushing teeth and replaced. It is important to wear the bands at all times so constant pressure is applied. Wearing them on and off can cause the teeth and jaw to ache more often.
With an overbite, typically the earlier the orthodontic treatment can start the better. If a patient is grinding their teeth and clenching their jaw, they are damaging their teeth. Some overbites make teeth cleaning difficult so the patient is at risk of tooth decay and gum disease.
A deep overbite is one of the longest orthodontic conditions to fix with braces. Often the overbite isn’t the only problem either. The patient is likely to have crooked teeth or overcrowding so there are multiple problems to work on.
Every case is different but for severe overbite cases braces could be needed for at least two years. Once the braces come off, a retainer is worn to keep the teeth in place.
Early treatment of children may include a palate expander to increase the size of the jaw to accommodate the crowded teeth in a small jaw. A larger jaw makes it an easier job for the braces to move teeth into the correct position and stops the need for removing teeth.
Parents most often recognise their child with an overbite has an orthodontic problem that needs attention. Children with an overbite will often come in earlier for treatment than other problems because they have health or psychological problems related to their teeth.
During sleep, a patient with an overbite may clench their jaw, or grind their teeth. This can cause joint pain and wear on the teeth. They may recommend a retainer worn at night to protect the teeth before the overbite problem is resolved.
Protruding front teeth are the most obvious orthodontic problem. Kids are cruel and it’s an easy taunt when their peer’s teeth are so noticeable. The bullying can cause serious self-esteem issues. Many parents request treatment as early as possible before their child’s peers tease them.
Someone with an overbite is at greater risk of damaging their teeth. When the top teeth protrude past the bottom, they can chip or be knocked out during sports, an accident or just being kids. Moving the front teeth back and fixing the overbite with braces ensures the teeth are more protected from knocks and falls.

The definition of a parrot mouth is when the top incisor teeth"s front edge is further forward that that of the lower teeth. Obviously there are all different degrees of parrot mouth — minor through to severe. In minor cases, the upper and lower incisors still meet, but are not perfectly aligned, but in severe cases, the two do not meet at all.
As far as genetics go, parrot mouth is NOT directly heritable. That is, we rarely see an individual sire or a mare throwing an abnormally high number of parrot mouthed foals. The most common cause of it is when a mare is bred to a stallion of very different head type. Surprisingly, these two stud animals often have normal teeth structure, yet when they are bred, the mismatch is so great that a parrot mouth offspring is produced.
It is important to remember that malocclusions in horse"s teeth (when they are not in the correct positioning and alignment etc) is poorly understood when it comes to how heritable it is, and is often a very complex mismatch of many genes. Thus having a badly conformed mouth in your animal may present a risk in breeding, but certainly doesn"t mean that animal will throw offspring with a similar condition.
The real problems with being parrot mouthed are due to the fact that horses" teeth are hypsodont teeth — that means that they have long crowns up in the bone and continue to erupt or move into the mouth throughout life — up to a point where there is no more tooth left to erupt into the mouth. If they are not opposing another tooth, they continue to erupt into the mouth to a point where they are a problem and dig into the opposite jaw etc.
Above: reserve crown of teeth allows the tooth, once fully formed and grown by around 6 years of age, to move into the mouth as the grinding surfaces of the teeth are worn away.
Horses" teeth do not grow indefinitely like rabbits" teeth, but for some time they continue to erupt into the mouth — with the purpose being to replace the tooth which is worn away during the chewing process. Because a paddock grazing horse may on average chew approximately 20 million times per year, the highly repeated grinding of tooth on tooth, or tooth onto fibrous feed material will lead to wearing away of the tooth. Thus new tooth needs to erupt into the mouth to replace the tooth which has been worn away. This tooth eruption process usually continues up until the horse is 15- 20 years of age — but sometimes more and sometimes less.
It is this fact that there is only so much tooth available to be used in a horse"s life, that the teeth — if normal height and angle,should NOT have their grinding surfaces ground smooth by an equine dental practitioner. Nature provided the horse with teeth made from three different substances — enamel, dentin and cementum — which all wear away at different rates. This produces a rough grinding surface which will effectively crush feed ready for digestion.Smoothing of the tooth"s grinding surface will often render a horse in pain and unable to chew its food properly for days to weeks — a very disturbing situation — especially for the horse!
Unless the tooth is abnormally high or the angle is wrong, the smoothing of a tooth"s grinding surface will reduce the life span of that tooth by at least 50 % if this procedure is repeated each year. What I am saying is not to be confused with the fact that the waste tooth eg sharp enamel points, tall teeth, hooks, waves, ramps, excessive transverse ridges etc, should not be removed or reduced at a dental visit.
The eruption process of teeth works fine if the teeth all line up even and oppose one another. But if they are not matched, then the tooth which is not opposed will continue to erupt into the mouth and become longer and longer.
As the elongating tooth or teeth become more prominent, they may cause the tooth to be moved or forced out of its normal position and they also may restrict the whole jaw"s normal RCM (rostro-caudal movement) whilst eating or when ridden.
As you can imagine, with 20 million chews per year, a hook on the upper first cheek tooth could result in that tooth being pushed forward away from the tooth behind it. Thus an abnormal gap in between the teeth would result, and feed becomes trapped in that gap, leading to rotting of the feed and severe gum disease (periodontal disease).
Periodontal disease is very common in horses, and needs to be detected early. If left untreated, it becomes irreversible, and often leads to premature loss of that tooth, and/or possible tooth root abscess formation. As those of you who have had meat stuck between your teeth for a few days, periodontal disease produces bad breath (halitosis) and can be quite painful. It may cause a horse to chew slowly, pack feed inside its cheeks (quid), drool saliva and tilt its head when eating etc.
The floating must be certain to address the associated overgrowths of teeth which arise and encourage the backwards displacement of the Mandible (jaw). These overgrowths include lipping of the incisors, hooks on the cheek teeth and excessive transverse ridges on the cheek teeth. Obviously the sharp enamel points must also be addressed.




 8613371530291
8613371530291